Letter from the Editor, Karen Schliep, PhD, MSPH, 2020
I am excited to introduce the 2020 issue of the Utah Women’s Health Review (UWHR), which was newly launched by the University of Utah Center of Excellence in Women’s Health and Spencer S. Eccles Health Sciences Library in May of 2020. Despite coming on board just as COVID-19 was ramping up in the US, we have had a successful past year. In May of 2020, we had a well-attended Sex, Gender, and Women’s Health Across the Lifespan symposium, featuring Dr. Susan Madsen updating us on the education, leadership, and well-being of Utah women; Dr. Lisa Diamond challenging us on new ways of thinking of sex, gender, transgender, and non-binary identities; Dr. Annie Fukushima painting the stark picture of gender-based violence across borders, and Dr. Marjorie Jenkins educating us on evidence-based clinical care for midlife women. And throughout the year, on a rolling basis, we published a variety of manuscripts and commentaries, several of which have been PubMed indexed due to being affiliated with NIH grants.
Our 2021 issue is well underway with an increasing number of submissions and publications. The journal publishes original research or review articles, data snapshots, and commentaries focusing on women’s health or sex and gender differences that affect the 7 Domains of Health—physical, social, emotional, intellectual, environmental, financial, and spiritual. The Editorial Board reflects our ONE U for U (1U4U) approach to sex and gender health. By creating and hosting this peer-reviewed journal within Eccles Library Digital Publishing, UWHR is able to facilitate publication opportunities to established sex and gender health researchers as well as graduate students, residents, and up-and-coming professionals all over Utah. UWHR’s rolling submissions and publication dates allow for a fast turn-around time as well as a satisfying experience for submitting authors. Using the WordPress platform, we invite ongoing submissions. There are no publication charges. All published articles are covered by a Creative Commons License (CC BY-NC-ND 4.0) and assigned a DOI. UWHR could not succeed without our valuable peer reviewers and associated editors. Please reach out to us if you are interested in serving in either of these capacities.
The broad spectrum of articles you will find in this 2020 issue highlight the reality that health is more than one dimension. Thinking of health in these multiple dimensions more accurately portrays women’s health challenges and embraces creative problem solving for improving women’s health across the lifespan. We look forward to receiving and reviewing your submissions this next year and beyond.
Sincerely,
Karen Schliep, PhD, MSPH
Editor-in-Chief
Exploring the Differences in Sleep Quality for Pre-Menopausal Women
Problem Statement
Sleep is an important consideration in a woman’s health: sleep disorders are associated with poor physical and mental health outcomes, including depression, anxiety, hypertension, cardiovascular disease, and glucose dysregulation1, and sleep also affects mood and brain cognition, including memory, decision making, sustained attention, and motor control.2 Compared to men, women experience a 40 percent increased risk in developing insomnia, and they report more sleepiness than men.3 Women’s sleep is affected by hormonal changes during menses, pregnancy, and menopause; social and environmental factors; and roles within the family. Healthcare and social work fields should address these unique challenges. With an 8:1 ratio of men to women observed in sleep centers,3 sleep in women is significantly understudied.
Status of the Literature
Della Monica et al. (2018) measured Rapid Eye Movement (REM) sleep in both men and women.2 The authors found that women have more sleep complaints and lower self-reported sleep scores, and they also experience higher levels of slow wave sleep (SWA) than men. This difference in subjective and objective sleep reports between men and women may be explained by a combination of social and cultural differences as well as biological and hormonal differences. More women are primary caregivers in their families than men, and women also constitute half of the workforce, which places considerable demands on women’s time.3 Women also experience higher levels of chronic conditions, such as overactive bladder, fibromyalgia, and chronic pain, which often cause a decrease in physical activity and poor sleep outcomes, but more research is needed to explore these connections.3
Women are particularly at risk for disrupted sleep during pregnancy and postpartum, which increases risk for poor mental health outcomes. For premenopausal women, poor sleep is linked to adverse reproductive health outcomes, such as menstrual irregularities, increased miscarriages, and lower birth rates.1 Richter et al. (2019) found that new mothers, especially first-time mothers, experienced worse sleep than new fathers, although fathers also reported a decrease in sleep quality.4 Sleep quality decreased for about three months postpartum, at which point sleep quality and duration often started to increase in quality and duration without, however, fully recovering even six years after giving birth.4 The study also found that breastfeeding is related to decreased sleep quality, yet this finding is inconsistent with past studies that reported no difference between breastfeeding or non-breastfeeding mothers. Regardless, becoming a parent is likely the most significant sleep-altering event for an individual and a major contribution to the overall decrease in sleep quality in adulthood.4
Social factors such as age, socioeconomic status, and dual vs. single parenting may affect sleep outcomes for pregnant or postpartum women. However, in the study conducted by Richter et al. (2019), there were no significant differences between wealthy, older mothers from a dual parenting home and their less wealthy, younger counterparts who were single parents.4
Call to Action
Sleep affects many aspects of health, including physical, mental, and social health, and should be addressed by social workers with their clients. Lack of sleep can significantly impact a woman’s life and her dual roles in the workforce and as a caregiver in her family.3 For social workers, it is especially important to address sleep with new mothers. This can include education on how sleep can affect physical and mental health during pregnancy and postpartum, discussing ways to improve sleep, and developing realistic expectations for sleep. While Richter et al. (2019) found that new mothers’ sleep will be affected regardless of socioeconomic status, age, and dual vs. single parenting, social workers should still emphasize resources to increase social and economic support.4 More broadly, we need additional research especially for sleep disorders among women and on the discrepancies between subjective and objective sleep outcomes, as sleep in women has historically been under-researched.
References
1. Kloss, J.D., Perlis, M.L, Zamzow, J. A., Culnan, E.J., & Gracia, C.R. (2015). Sleep, sleep disturbance, and fertility in women. Sleep Medicine Reviews 22, 78–87. doi:10.1016/j.smrv.2014.10.005
2. della Monica, C., Johnsen, S., Atzori, G., Groeger, J. A., & Dijk, D.-J. (2018). Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20–84 years. Frontiers in Psychiatry 9, 255. doi:10.3389/fpsyt.2018.00255
3. Mallampalli, M. P., & Carter, C. L. (2014). Exploring sex and gender differences in sleep health: A society for women’s health research report. Journal of Women’s Health, 23(7), 553–562. doi:10.1089/jwh.2014.4816
4. Richter, D., Kramer, M. D., Tang, N. K. Y., Montgomery-Downs, H. E., & Lemola, S. (2019). Long-term effects of pregnancy and childbirth on sleep satisfaction and duration of first-time and experienced mothers and fathers. SLEEP, 42(4). doi:10.1093/sleep/zsz015
Citation
Morazan A (2021). Exploring the Differences in Sleep Quality for Pre-Menopausal Women. Utah Women’s Health Review. doi: https://doi.org/10.26054/0D-F0VN-HZM4
Hidden Women: Unmet Medical Needs of Utah’s Incarcerated Women
Problem Statement
In this commentary we will outline the unique health needs of Utah’s imprisoned female population, including the need to address cervical and breast cancer, age-related illness, substance abuse, and heart disease.
We highlight that incarcerated women experience higher rates of substance abuse, physical and sexual assault, and trauma than their non-incarcerated counterparts, leading to a greater need for specialized medical attention.
We will outline how Utah’s above-average rates of imprisoned women require more specialized and preventative healthcare. We further argue for greater research and advocacy for this marginalized population, which is hidden from the public eye.
We use the seven domains of women’s health as a framework to argue for a whole-health approach to the overall wellness for this population.
Status of the Literature
The rates of incarcerated women across the United States are vast when compared to other developed nations. Currently the United States “lock[s] women up at rates that are at least 5 times the rates of our closest international allies.”1 The rate of women in prisons across the country is growing faster than that of imprisoned men.2 The current system was built for men and falls short in addressing women’s unique biological and psychosocial needs.
The population in U.S. women’s prison is overwhelmingly made up of nonviolent drug offenders. The complex nature of women’s experiences of trauma creates a unique and desperate need for tailored interventions that address the overall health of this population.3 Women who are or have been incarcerated are less likely to have medical insurance, preventative healthcare, financial resources, and have lower levels of education.4 Marginalized groups such as incarcerated women, of whom many also belong to a racial minority, experience higher rates of oppression that lead to worse health outcomes,5 including chronic illness and infectious diseases.6
Women who are incarcerated are four to five times more likely to have cervical cancer compared to women without criminal histories. Although more research must be done, some studies suggest that imprisoned women are also several times more vulnerable to mortality due to cervical cancer.7 Research has shown that one contributing factor to the increased cervical cancer risk is low health literacy. Ramaswamy implemented brief but effective education interventions that improved health literacy. Education is intended to supplement advocacy, prevention services including cancer screenings, and resources for health insurance as women re-enter their communities.4
“The limited studies evaluating the health of older female inmates indicate that, like older male inmates, older female inmates are generally sicker than their non-incarcerated counterparts.”8 Female inmates over 55 have higher rates of hypertension, arthritis, and respiratory disease compared to non-imprisoned women over 65. Older women inmates also have higher rates of chronic illness than their male counterparts.8
Call to Action
Little progress has been made in changing legislation to increase incarcerated women’s access to medical care. In 2019, Utah lawmakers passed a bill to ban shackling inmates during birth and allocated funds for reproductive health education for incarcerated women.9 We could find no Utah law or code that dictated regular preventative screening methods for cervical cancer or other conditions that affect women over the lifespan. The Utah Prisoner Advocate Network reported that “hormones and gynecological attention [are] reported to be offered for women’s concerns in Draper at the Wasatch Infirmary.10 There were no other mentions of required preventative procedures or screening except for when an inmate is first admitted to the facility.
The limited demographic data for Utah’s incarcerated women’s population presents a barrier to providing appropriate healthcare resources. Without detailed data, it is difficult to understand the full scope of health issues imprisoned women face. More research and information are required to implement evidence-based interventions. It is important to recognize how the seven domains of health—physical, social, financial, environmental, intellectual, spiritual, mental—are intertwined for this marginalized population.11 Better, more complete demographic data are needed to motivate legislation changes to meet the unique needs of female inmates in Utah.
References
1. Kajstura, A. (2018). States of women’s incarceration: The global context2018. Prison Policy Initiative. Retrieved 08 July, 2021, from https://www.prisonpolicy.org/global/women/2018.html
2. Minton T. D., Ginder S., Brumbaugh S. M., Smiley-McDonald, H., & Rohloff, H. (2015). Census of jails: Population changes, 1999–2013. US Department of Justice. Office of Justice Programs. Retrieved 08 July, 2021, from https://www.bjs.gov/content/pub/pdf/cjpc9913.pdf
3. National Commission on Correctional Health Care Position Statement. (2005). Journal of Correctional Health Care, 11(4), 381-389. doi: 10.1177/107834580401100407
4. Ramaswamy, M., Lee, J., Wickliffe, J., Allison, M., Emerson, A., & Kelly, P. J. (2017). Impact of a brief intervention on cervical health literacy: A waitlist control study with jailed women. Preventive Medicine Reports, 6, 314–321. doi:10.1016/j.pmedr.2017.04.003
5. Ledesma, E., & Ford, C. L. (2020). Health implications of housing assignments for incarcerated transgender Women. American Journal of Public Health, 110(5), 650–654. doi:10.2105/AJPH.2020.305565
6. Timko, C., Johnson, J. E., Kurth, M., Schonbrun, Y. C., Anderson, B. J., & Stein, M. D. (2019). Health services use among jailed women with alcohol use disorders. Journal of Behavioral Health Services & Research, 46(1), 116–128. doi:10.1007/s11414-018-9634-7
7. Kouyoumdjian F. G., McConnon A., Herrington E. R. S., Fung K., Lofters A., & Hwang S. W. (2018). Cervical cancer screening access for women who experience imprisonment in Ontario, Canada. JAMA Netw Open;1(8) doi:10.1001/jamanetworkopen.2018.5637
8. Barry, L. C., Adams, K. B., Zaugg, D., & Noujaim, D. (2019). Health-care needs of older women prisoners: Perspectives of the health-care workers who care for them. Journal of Women & Aging, 32(2), 183202. doi:10.1080/08952841.2019.1593771
9. Jacobs, B. (2019, July 26). Utah lawmakers paid more attention to incarcerated women this year. The Salt Lake Tribune. https://www.sltrib.com/news/2019/07/26/utah-lawmakers-paid-more/
10. Utah Prisoner Advocate Network. (2020). Medical care and infirmaries (Draper and Gunnison prison). Retrieved July 08, 2021, from https://utahprisoneradvocate.org/prisoner-family- 101/medical-info/
11. Frost, C. J. & Digre, K. B. (Eds). (2016). The 7 domains of health: Multidisciplinary considerations of women’s health in the 21st century. Kendall Hunt Publishers.
Citation
Fuhriman C, Hill K, and Martin A (2021). Hidden Women: Unmet Medical Needs of Utah’s Incarcerated Women. Utah Women’s Health Review. doi: https://doi.org/10.26054/0D-NQ3T-8WYK
The Impact of Socioeconomic Status on Women’s Physical Health
Problem Statement
The relationship between socioeconomic status (SES) and women’s physical health warrants further study, particularly through a social work lens. SES is determined by more than income; SES is also influenced by one’s level of education, individual perceptions of social standings, and overall financial security. A lower SES increases the likelihood that one will develop physical and mental health issues over the course of the lifetime.1 With low SES influencing women’s education and social standings, the increased risk warrants further research into the impacts these detriments have on women specifically through a social work lens.
Women are already at greater risk for experiencing various forms of systemic and institutional discrimination. Wang and Geng (2019) found that those with a low SES are more likely to experience a decline in exercise and quality of sleep, and an increase in substance use.2 Kivimäki et al. (2020) suggest that numerous unhealthy lifestyle choices are related to socioeconomic disadvantage.1 Further, lower SES is correlated with poor self-reported health outcomes and lower life expectancies.3 While these findings are not exclusive to women, low SES is one of many compounding factors that are detrimental to a woman’s health and wellbeing. Social work is hallmarked by a commitment to promoting the wellbeing of all people with an emphasis on marginalized populations. Additional research on the relationship between women’s physical health and SES could open new pathways for further study, advocacy, and service implementation within the range of social work contexts.
Status of the Literature
The literature on the impacts of socioeconomic status on women’s physical health is fairly extensive; however, there is a dearth of articles exploring direct implications for social work practice. Lower SES and the experience of poverty are major factors influencing physical health outcomes for women. Lower income and wage inequality can contribute to a multitude of negative physical health outcomes for women, sometimes even leading to premature death.4 The interrelated, cyclical nature of lower SES, less education, poverty, and various health issues is largely overlooked in literature when examining the impacts on women specifically. Income disparities based on gender continue to exist in the United States. Such disparities create further difficulties for women seeking access to resources and services that promote their physical wellbeing. Women belonging to marginalized populations experience the compounded effects of various institutional, systemic, and cultural barriers. Many of the resources and forms of assistance that individuals of low SES seek are rendered necessary because of the barriers imposed by poverty itself. Additionally, lower SES and poverty often create interpersonal challenges for women which also impact physical health.
Interpersonal violence (IPV) and abuse have major impacts on women’s overall physical health. Rates of IPV are higher among minoritized, undocumented, and lower SES women, posing a major risk to their physical health. Physically abusive relationships often impact women’s daily functioning due to increased rates of broken bones, diseases, chronic disorders, and gynecological problems. In addition to these risks, women experiencing IPV and abuse are at increased risk of substance abuse or becoming suicidal.5 Exploring the connections between SES, IPV, and physical health in women in the context of social work practice holds the potential for vast improvements in service delivery and subsequent outcomes.
Call to Action
Social workers serve many clients of low SES across various populations. It is critical that social workers recognize the profound impacts of low SES on women’s physical health. Promoting and engaging in evidence-informed practice and practice-informed research are ethical responsibilities integral to good social work practice. Doing so is essential for the betterment of those seeking direct services and, subsequently, wider society.
Continued research into the relationship between women’s socioeconomic status, poverty, and physical health will allow for increased understanding and improved quality of care. East & Roll (2015) recommend that social workers in clinical and community settings better recognize how gender-based inequalities impact the women they work with;6 however, additional research into the larger impacts that low SES has on women’s physical health and overall wellbeing can benefit all those who work with women and their loved ones. Understanding systemic barriers that women face allows social workers, and other professionals, to operate more efficiently in their work on the micro, mezzo, and macro levels. Additional research on the connection between women’s physical health and SES through the lens of social work practice will benefit clients and professionals alike.
References
1. Kivimäki, M., Batty, G. D., Pentti, J., Shipley, M. J., Sipilä, P. N., Nyberg, S. T., … & Marmot, M. G. (2020). Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. The Lancet Public Health, 5(3), e140-e149.
2. Wang, J., & Geng, L. (2019). Effects of Socioeconomic Status on Physical and Psychological Health: Lifestyle as a Mediator. International journal of environmental research and public health, 16(2), 281. https://doi.org/10.3390/ijerph16020281
3. Arpey, N. C., Gaglioti, A. H., & Rosenbaum, M. E. (2017). How Socioeconomic Status Affects Patient Perceptions of Health Care: A Qualitative Study. Journal of Primary Care & Community Health, 169–175. https://doi.org/10.1177/2150131917697439
4. Gilroy, H., Nava, A., Maddoux, J., Mcfarlane, J., Symes, L., Koci, A., & Fredland, N. (2014). Poverty, Partner Abuse, and Women’s Mental Health: New Knowledge for Better Practice. Journal of Social Service Research, 41(2), 145–157. https://doi.org/10.1080/01488376.2014.972010
5. Vil, N. M., Sabri, B., Nwokolo, V., Alexander, K. A., & Campbell, J. C. (2016). A Qualitative Study of Survival Strategies Used by Low-Income Black Women Who Experience Intimate Partner Violence. Social Work, 62(1), 63-71. doi:10.1093/sw/sww080
6. East, J. F., & Roll, S. J. (2015). Women, Poverty, and Trauma: An Empowerment Practice Approach. Social Work, 60(4), 279-286. doi:10.1093/sw/swv030
Citation
Powell DK, Lockyer CA, and Broadbent JG (2021). The Impact of Socioeconomic Status on Women’s Physical Health. Utah Women’s Health Review. doi: https://doi.org/10.26054/0D-T66J-A0ZE
Obesity and Mental Health
Problem Statement
The prevalence of obesity in the United States has increased from 30.5% to 42.4% among adults over the past twenty years.1 Although obesity has an impact on health regardless of gender, some disparities exist. Rates of obesity are similar among men and women; however, stroke risk associated with obesity has remained stagnant in men and increased three-fold in women since the year 2000.2 In a sample of 682 people with comorbid binge-eating disorder and obesity, women had significantly higher eating disorder psychopathology than men.3 This suggests that obesity in women may have a psychological manifestation that varies from that of men. In a systematic review of the link between adverse life experiences and obesity and binge-eating, 85% of available studies found a positive association between trauma and obesity, and 90% of the studies found a positive association between trauma and binge-eating disorder.4 Yet, the Centers for Disease Control and Prevention (CDC) guidelines for weight loss and obesity prevention include nutrition and exercise strategies but make no mention of psychological interventions to address obesity.5 Why aren’t we addressing the psychological component of obesity?
Status of Literature
Recent literature confirms previous research that those with obesity are, in fact, at higher risk of experiencing eating disorders. To improve the care provided to those with obesity, a greater exchange of experiences and specialized knowledge between healthcare professionals working in the obesity field and those working in the field of eating disorders is needed.6 In 2018, a team of researchers set out to examine the role stress management/mental health coaching plays in the treatment of obesity.7 Two groups underwent a weight loss program at an obesity clinic. One group received stress management courses in addition to the weight loss program. At the end of eight weeks, the group who received stress management exhibited greater weight loss and decreased depression and anxiety. As more information is discovered about the benefits of psychological treatment for obesity, various forms of psychological treatment are being examined. In 2017, another team of researchers found Cognitive Behavior Therapy for individuals with obesity to be effective and a preferred method for obesity treatment.8
Currently, the COVID-19 pandemic is having negative impacts on weight gain and eating disorders. Researchers are seeing that many individuals are gaining weight as a result of the COVID-19 pandemic.9 In addition to weight gain, COVID-19 has negatively impacted those with eating disorders. Studies show that those with bulimia nervosa and binge-eating disorders reported experiencing more episodes of binge eating and more compulsion to binge eat.10 We expect to see this COVID-19 increase in obesity and eating disorders proportionally higher in women compared to men. With the obesity and mental health link ever-present, we are in urgent need of obesity healthcare reform.
Call to Action
A recent review of current treatments for obesity include lifestyle changes in diet and exercise, pharmacotherapeutic interventions, and surgical interventions as the primary treatment options.11 None of these interventions explicitly address psychological barriers to care associated with obesity. Not only in the wake of COVID-19 but with the perpetrating growth of the obesity epidemic, emerging studies reflecting the importance of incorporating psychological treatments in current weight loss programs need to be implemented. To better address the obesity epidemic, more research needs to be conducted related to understanding and treating the psychological aspects of obesity, including its comorbidity with binge eating disorder and its correlation with experiences of trauma.
References
1. Hales, C. M., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2020). Prevalence of obesity and severe obesity among adults: United States 2017-2018. NCHS Data Brief No. 360. National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db360.htm
2. Towfighi, A., Zheng, L., Ovbiagele, B. (2010). Weight of the obesity epidemic: Rising stroke rates among middle aged women in the United States. Stroke, 41(7). https://doi.org/10.1161/STROKEAHA.109.577510
3. Lydecker, J. A., & Grilo, C. M. (2018). Comparing men and women with comorbid binge-eating disorder and obesity. International Journal of Eating Disorders, 51(5), 411-417. https://doi.org/10.1002/eat.22847
4. Palmisano, G. L., Innamorati, M., & Vanderlinden, J. (2016). Life adverse experiences in relation with obesity and binge eating disorder: A systematic review. Journal of Behavioral Addictions, 5(1), 11-31. https://doi.org/10.1556/2006.5.2006.018
5. Centers for Disease Control and Prevention [CDC]. (2020). Healthy weight, nutrition, and physical activity. https://www.cdc.gov/healthyweight/losing_weight/index.html
6. Luz, F. D., Hay, P., Touyz, S., & Sainsbury, A. (2018). Obesity with Comorbid Eating Disorders: Associated Health Risks and Treatment Approaches. Nutrients, 10(7), 829. doi:10.3390/nu10070829
7. Xenaki, N., Bacopoulou, F., Kokkinos, A., Nicolaides, N. C., Chrousos, G. P., & Darviri, C. (2018). Impact of a stress management program on weight loss, mental health and lifestyle in adults with obesity: a randomized controlled trial. Journal of molecular biochemistry, 7(2), 78–84.
8. Castelnuovo G, Pietrabissa G, Manzoni GM, Cattivelli R, Rossi A, Novelli M, Varallo G, Molinari E. Cognitive behavioral therapy to aid weight loss in obese patients: current perspectives. Psychol Res Behav Manag. 2017 Jun 6;10:165-173. doi: 10.2147/PRBM.S113278. PMID: 28652832; PMCID: PMC5476722.
9. Todisco, P., & Donini, L. M. (2020). Eating disorders and obesity (ED&O) in the COVID-19 storm. Eating and Weight Disorders – Studies on Anorexia, Bulimia and Obesity. doi:10.1007/s40519-020-00938-z
10. Robertson, S. (2020, June 01). COVID-19 negatively impacts people with eating disorders. Retrieved November 30, 2020, fromhttps://www.news-medical.net/news/20200601/COVID-19-negatively-impacts-people-with-eating-disorders.aspx
11. Ruban, A., Stoenchev, K., Ashrafian, H., & Teare, J. (2019). Current treatments for obesity. Clinical Medicine, 19(3), 205-212. https://doi.org/10.7861/clinmedicine.19-3-205
Citation
Taylor E, Bak A, and Moore P (2021). Obesity and Mental Health. Utah Women’s Health Review. doi: 10.26054/0D-0VMK-H441
Female Healthcare Workers’ Mental Health During COVID-19 and Available Resources
Problem Statement
Adverse mental health outcomes are a severe public health issue that significantly affects our healthcare providers’ health and performance.1 Worldwide, female healthcare providers have been physically and emotionally exhausted from caring for COVID-19 patients. Their mental health may be affected by the increased demand for care and the maintenance of personal responsibilities. Additional resources must be made available to care for healthcare providers’ mental health during the COVID-19 pandemic.
Status of Literature
Burnout is a familiar syndrome among healthcare providers manifested by symptoms of spiritual and emotional exhaustion, depersonalization, and a decreased sense of personal achievement.2 Burnout contributes to insomnia, headaches, reduced job satisfaction, and increased mental health problems such as depression and anxiety.3 Evidence of burnout was reported in 42% of 15,000 US physicians from a 2018 survey, which is associated with an increased risk of significant medical errors.4
Women typically have the burden of child and family care, however, family resources were shut down by the pandemic. Mothers and wives in our community who are also our healthcare providers are unfairly affected emotionally and physically by the global pandemic. The global pandemic has demanded much more of our physicians, nurses, and other healthcare providers, contributing to burnout. These challenges include the pressure of reducing the spread of infection, developing suitable short-term and long-term strategies and plans, continuing to treat non-COVID patients successfully, and maintaining personal and family responsibilities.5 Healthcare providers report more distress about family contracting COVID-19 or unknowingly infecting others than acquiring themselves.6 These conditions for our female health care workers are exasperated by the lack of or ineffectiveness of available resources.
Research indicates that female health care workers are at increased risk for mental health problems during the current COVID-19 pandemic.7 The recent literature has demonstrated a higher risk for anxiety, depression, and greater fear in medical staff with direct contact with COVID-19 patients.5 Healthcare providers on the frontlines of COVID-19 (i.e., emergency department, intensive care, and infectious disease units) are at greater risk for psychological disorders.8,9 Older healthcare providers have demonstrated increased stress related to a lack of personal protective equipment and longer work hours.10 Additionally, women and individuals in high-risk areas may have more negative psychological health outcomes.11 A study concluded that more attention needs to be given to female nursing staff’s mental health between the ages of 30-39.12
Call to Action
Female healthcare providers working on the front lines during the COVID-19 pandemic have been overwhelmed with providing care for the public. During our current COVID-19 pandemic or any future national crisis, our female healthcare providers should be aware of the available resources and aid offered by their employer and others within the community. As an interdisciplinary team of social work and public health, we offer the following information in hopes of informing healthcare providers of available relief and ameliorate stress.
Intermountain Healthcare (IHC) provided mental health counseling for physicians and an employee assistance hotline with other resources and help for all employees.13 IHC also offered clean scrubs for their physicians to wear home after a shift to avoid the risk of infecting family members; however, this service was not offered to nurses and MAs. As the provision of clean scrubs and PPE may have relieved stress and anxiety, we believe in the inclusion of all employees to receive clean scrubs. In addition, IHC offered “COVID” pay up to 2 weeks for employees who became infected with COVID-19 or had to self-quarantine. The following resources were offered on the IHC website (2020), under the headings “Caregiver Resources for COVID-19”, “COVID Related Caregiver Discounts,” and “Employee Assistance Program” and were available for all healthcare providers who are giving care during the global pandemic.14, 15
Nevertheless, it is unknown how well these resources are publicized to and utilized by employees. We propose increased emphasis and advertisement on mental health resources available to aid those that are risking their physical and mental health to care for others. Additionally, increased monetary compensation or PTO may be beneficial in improving job satisfaction and mental health among healthcare providers. Aside from health measures, our best defense against COVID-19 is providing optimal conditions and comprehensive resources for our healthcare providers.
References
1. Shaukat, N., Ali, D.M. & Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med 13, 40 (2020). https://doi.org/10.1186/s12245-020-00299-5
2. Papathanasiou I. V. (2015). Work-related Mental Consequences: Implications of Burnout on Mental Health Status Among Health Care Providers. Acta informatica medica : AIM : journal of the Society for Medical Informatics of Bosnia & Herzegovina : casopis Drustva za medicinsku informatiku BiH, 23(1), 22–28. https://doi.org/10.5455/aim.2015.23.22-28
3. Salyers, M., Bonfils, K., Luther, L., Firmin, R., White, D., Adams, E., & Rollins, A. (2016). The relationship between professional burnout and quality of safety in healthcare: A meta-analysis. Journal of General Internal Medicine, 32, 475-482.
4. Yates, S.W. (2020). Physician stress and burnout. The American Journal of Medicine, 133,(2), 160-164.
5. Shreffler, J., Petrey, J., & Huecker, M. (2020). The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. The Western Journal of Emergency Medicine, 21(5), 1059–1066. https://doi.org/10.5811/westjem.2020.7.48684.
6. Barzilay, R., Moore, T.M., & Greenberg, D.M.(2020). Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry 10(291) https://doi.org/10.1038/s41398-020-00982-4
7. Liu, S., Yang, L., Zhang, C., Xu, Y., Cai, L., Ma, S., Wang, Y., Cai, Z., Du, H., Li, R., Kang, L., Zheng, H., Liu, Z., Zhang, B. (2021). Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. Journal of Psychiatric Research, 137(0022-3956)393-400. https://doi.org/10.1016/j.jpsychires.2021.03.014.
8. Liu, C. Y., Yang, Y. Z., Zhang, X. M., Xu, X., Dou, Q. L., Zhang, W. W., & Cheng, A. (2020). The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology and infection, 148, e98. https://doi.org/10.1017/S0950268820001107
9. Lu, W., Wang, H., Lin, Y., & Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research, 288, 112936. https://doi.org/10.1016/j.psychres.2020.112936North Face. (n.d.).
10. Guo, J., Liao, L., Wang, B., Li, X., Guo, L., Tong, Z. Guan, Q., Zhou, M., Wu, Y., Zhang, J. & Gu, Y. (2020). Psychological Effects of COVID-19 on Hospital Staff: A National Cross-Sectional Survey of China Mainland. Available at SSRN 3550050.
11. Zhu, Z., Xu, S., Wang, H., Liu, Z., Wu, J., Li, G., Miao, J., Zhang, C., Yang, Y., Sun, W., Zhu, S., Fan, Y., H. J., Liu, J., & Wang, W. (2020). COVID-19 in Wuhan: Immediate Psychological Impact on 5062 Health Workers. MedRxiv.
12. Alateeq, D., Aljhani, S., Althiyabi, I., & Majzoub, S. (2020). Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. Journal of Infection and Public Health, 13(0), 1432-1437.
13. Caregiver Resources for COVID-19. (2020). Retrieved November 16, 2020, from https://intermountainhealthcare.org/covid19-coronavirus-for-healthcare-professionals/caregiver-resources/
14. Employee Assistance Program (2020). Retrieved November 19, 2020, from https://intermountainhealthcare.org/services/employee-assistance-program/services/
15. COVID-Related Caregiver Discounts. (2020). Retrieved November 16, 2020, from https://intermountainhealthcare.org/covid19-coronavirus-for-healthcare-professionals/caregiver-resources/discounts/
Citation
Ryan H and Homer L (2021). Female Healthcare Workers’ Mental Health During COVID-19 and Available Resources. Utah Women’s Health Review. doi: 10.26054/0D-NHJB-QAD4
Extreme Risk Protective Orders and Reducing Intimate Partner Homicides
Problem Statement
Domestic violence (DV) and intimate partner violence (IPV) range from physical, emotional, sexual, mental, and verbal abuse from either a person in the same domestic household of a person or a person who wants to be intimate with another person. DV and IPV can have lasting consequences on a woman’s health, including emotional trauma, lasting physical injuries, and chronic pain, and even death.1 Statistics show that having guns in a household increases the perpetrator’s possibility of using a firearm in their violence towards a victim. Almost half of the adult homicides per year are from DV situations, and often guns are the weapon of choice.2
Status of Literature
Utah has had a higher rate of DV compared to national rates. Nationally one in four women will experience DV or IPV in their lifetime, and in Utah, one in three will experience DV or IPV.2 The repercussions of DV are significant. 42% of adult homicides since 2000 in Utah have been related to DV, children witness 22% of DV homicides, and guns are commonly the weapon of choice for male perpetrators in DV homicide.2 Understanding these statistics is even more critical today because many people, including Utahns, have been more isolated and at home with abusive partners due to COVID-19. Evans (2020) is calling for additional research around the impact of COVID-19 and increasing DV rates. However, anecdotally, there appears to be higher rates of DV due to many of the COVID-19 restrictions ranging from social distancing, isolation, quarantine, and shelter in place.3 When we can understand the impact of the COVID-19 and DV, we can provide better services and programs to support victims.
With over 70% of female homicides in Utah being related to domestic violence, concerns about providing more protection for women is an essential part of social policy legislation.4 Individuals experiencing domestic violence are often at high risk of death by intimate partner homicide. In homes where domestic violence is occurring, the presence of a firearm in the home increases the risk of a woman being murdered by their male intimate partner to 500%.5 Furthermore, 50% of all intimate partner homicides were committed with a gun, indicating that guns are the primary weapon used in intimate partner homicides.5
Call to Action
The Violence Against Women Act (VAWA) addresses individuals convicted of domestic violence and the possession of a firearm, but there is no language about relinquishing firearms.5 Ultimately, gun ownership is considered a state’s right, and Utah’s recent legislative session passed H.B. 229, marketing the bill as a suicide prevention act, including specific language about a requirement to relinquish firearms.6 The law requires that individuals have the option of surrendering firearms to law enforcement when the protective order is served or within 24 hours to a federally licensed firearms dealer.6 Although this does provide relinquishment language, there is a significant gap of 24 hours where a domestic violence victim could be murdered by their partner before turning their guns in. Furthermore, the law doesn’t include specific language for victims of domestic violence. The best way for concerned community members to support extreme risk protective orders is to reach out to local legislators to make sure Utah’s extreme risk protective orders include specific language about relinquishment of firearms in cases of DV and IPV, as well as require that firearms are surrendered only and immediately when the order is served to the respondent. In addition, people in Utah can work with UDVC to ensure that DV and IPV victims can have the protection and safety they deserve especially during the times of national crisis. Such as our current COVID-19 pandemic, when many legal processes and hearings are becoming delayed.
References
1. Frost, C., & Digre, K. (2016). 7 domains of women’s health: Multidisciplinary considerations of women’s health in the 21st century (1st ed., pp. 1-224). Dubuque, IA: Kendall Hunt Publishing.
2. Utah Domestic Violence Coalition (UDVC). (2016). UDVC Facts Sheet. Policy & Reports. Retrieved +December 1, 2020, from https://www.udvc.org/resources/policy-reports/reports.html
3. Evans, D. P. (2020). COVID-19 and violence a research call to action. BMC Women’s Health 20, 249. https://doi.org/10.1186/s12905-020-01115-1
4. Utah Department of Health. (2019). Domestic violence fatalities in Utah: 2003-2008 (pp.1-48). Salt Lake City, UT: Violence and Injury Prevention Program.
5. Díez, C., Kurland, R., Rothman, E., Bair-Merritt, M., Fleegler, E., & Xuan, Z. et al. (2017). State intimate partner violence-related firearm laws and intimate partner homicide rates in the United States, 1991 to 2015. Annals Of Internal Medicine, 167(8), 536. doi: 10.7326/m16-2849
6. Utah Legislature, H.B. 229 Extreme Risk Protection Order§ 78B-7-604(5), (2020) Retrieved from https://le.utah.gov/~2020/bills/static/HB0229.html
Citation
Freed S and Coffey R (2021). Extreme Risk Protective Orders and Reducing Intimate Partner Homicides. Utah Women’s Health Review. doi: 10.26054/0D-WGNC-36WX
Mental Health for Latina Youth: The Need for Tailored Resiliency Interventions
Problem Statement
Mental health is a serious issue associated with reduced life satisfaction, shortened life expectancy, and higher rates of physical illnesses.1,2 Among adolescents, poor mental health significantly impacts long-term health behaviors, such as drug use or sexual behaviors.3 In the recent Youth Risk Behavior Survey Data Summary and Trends Report for 2019, feelings of hopelessness and sadness increased among adolescents from 2009-2019 by 10% .4 The mental health and life outcomes of Latina adolescents is of particular concern as they have an increased risk of mental illness due to challenging experiences such as discrimination, violence, language and cultural barriers, academic challenges, and a lack of support.5,6 It is apparent that current programs and interventions do not meet the health needs of Latina adolescents as adolescent females reported feelings of sadness or hopelessness by almost double the percentage of adolescent males, and 40% of Hispanic students reported these feelings compared to 36% of White students and 32% of Black students.4 In an attempt to address these challenges and improve mental health outcomes, researchers have implemented several resiliency programs among immigrant and U.S.-born Latina/o adolescents, with the hope that resilience will strengthen their ability to adapt to change and deal successfully with life’s challenges.7 However, these resiliency programs often fail to account for differences in sex and gender (sex referring to biological characteristics and gender referring to personal identification) among Latino and Latina adolescents. This is a potential issue as researchers have found that sex and gender play a significant role in Latina adolescents’ future mental and physical health outcomes.8 Despite the overall success of resilience programs, without gender- and sex-specific research, many programs are likely inadequate in meeting the needs of Latina youth.
Status of Literature
In general, many types of programs exist to help develop and encourage resilience among youth. The first of these focuses on parenting. Studies have shown that effective parenting can prevent long-term adverse outcomes among children in many areas of life, such as substance use, mental health, physical health, and academics. A review of experimental parenting studies found that out of 22 programs reviewed, 20 had a significant impact on long-term outcomes up to 15 years after participation.9 School-based interventions have also been effective at increasing resilience. One such school program implemented a curriculum to help adolescents identify emotions and the appropriate response to emotions. Results showed that the curriculum was helpful, enhanced support and connection, and destigmatized mental health.10 Another common resilience intervention is mindfulness training. Mindfulness uses meditation to focus one’s mind on the present moment and teaches individuals how to regulate emotions. Researchers implemented one mindfulness program among Asian and Latina/o minority adolescents. Participants were randomized to take a 12-week training course either during the first or second semester of school. Results showed that the program reduced perceived stress, expressive suppression, avoidance and fusion, rumination, internalizing problems, externalizing problems, and attention problems.11 The last commonly used resilience intervention is a community-based approach. This involves studying the ecological factors surrounding an individual and responding appropriately to improve overall living conditions.12 One study found that resiliency programs often overlook structural barriers to resilience, even though understanding these barriers is crucial to the successful development of resilience.13
Currently, researchers have tailored only one resilience program to fit Latina youth. This program is known as Positive Youth Development (PYD). PYD emphasizes personal agency and focuses on youths’ strengths as a way to confront challenges.14 Researchers have used PYD to address various challenges faced by Latina youth, such as sexual identity, ethnic discrimination, and incarceration.15, 16 One study showed that PYD effectively strengthened resiliency attitudes and skills such as humor or creativity, measured through the use of the Resiliency Attitudes and Skills Profile (RASP).16
Call to Action
Researchers argue that minority females are frequently confronted with experiences of adversity and gender-based discrimination, requiring them to develop resilience .17 However, much of the literature on resilience among Latina/o adolescents is limited by not considering sex and/or gender differences.15 This limits the effectiveness of the programs and the subsequent development of resilience for Latina adolescents. Sex- and gender-specific research is needed to explore the impact that existing resilience programs have on Latina adolescents. Health professionals will then be able to refine resilience programs to better serve Latina adolescents. This could significantly improve their future mental and physical health outcomes.8
References
1. Fergusson, D. M., Mcleod, G. F. H., Horwood, L. J., Swain, N. R., Chapple, S., & Poulton, R. (2015). Life satisfaction and mental health problems (18 to 35 years). Psychological Medicine. https://doi.org/10.1017/S0033291715000422
2. Happell, B., Platania-Phung, C., Fellow Stephanie Webster, R., Scott, D., & Fellow, R. (2015). Applying the World Health Organization Mental Health Action Plan to evaluate policy on addressing co-occurrence of physical and mental illnesses in Australia. Australian Health Review, 39, 370–378. https://doi.org/10.1071/AH14098
3. Centers for Disease Control and Prevention. (2021). Mental health. https://www.cdc.gov/healthyyouth/mental-health/index.htm
4. Centers for Disease Control and Prevention. (2019). Youth risk behavior survey data summary & trends report: 2009-2019. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/YRBSDataSummaryTrendsReport2019-508.pdf
5. Diaz, Y., & Fenning, P. (2017). Toward understanding mental health concerns for the latinx immigrant student: A review of the literature. Urban Education. https://doi.org/10.1177/0042085917721953
6. Rodriguez, C., & Ballesteros, C. (2019). Acculturation among Latinx youth and ways to best support their social emotional wellbeing in the school environment. http://dspace.calstate.edu/handle/10211.3/210186
7. Peña, C., Jones, L., Orange, A., Simieou, F., & Márquez, J. (2018). Academic success and resiliency factors: A case study of unaccompanied immigrant children. American Journal of Qualitative Research, 2(1), 162–181. http://www.ajqr.org/
8. Sanchez, D., Vandewater, E. A., & Hamilton, E. R. (2019). Examining marianismo gender role attitudes, ethnic identity, mental health, and substance use in Mexican American early adolescent girls. Journal of Ethnicity in Substance Abuse, 18(2), 319–342. https://doi.org/10.1080/15332640.2017.1356785
9. Sandler, I., Ingram, A., Wolchik, S., Tein, J.-Y., & Winslow, E. (2015). Long-term effects of parenting-focused preventive interventions to promote resilience of children and adolescents. Child Development Perspectives, 9(3), 164–171. https://doi.org/10.1111/cdep.12126
10. Ijadi-Maghsoodi, R., Marlotte, L., Garcia, E., Aralis, H., Lester, P., Escudero, P., & Kataoka, S. (2017). Adapting and implementing a school-based resilience-building curriculum among low-income racial and ethnic minority students. Contemporary School Psychology, 21(3), 223–239. https://doi.org/10.1007/s40688-017-0134-1
11. Fung, J., Kim, J. J., Jin, J., Chen, G., Bear, L., & Lau, A. S. (2019). A randomized trial evaluating school-based mindfulness intervention for ethnic minority youth: Exploring mediators and moderators of intervention effects. Journal of Abnormal Child Psychology, 47(1), 1–19. https://doi.org/10.1007/s10802-018-0425-7
12. Shaw, J., McLean, K. C., Taylor, B., Swartout, K., & Querna, K. (2016, January 1). Beyond resilience: Why we need to look at systems too. Psychology of Violence, Vol. 6, pp. 34–41. https://doi.org/10.1037/vio0000020
13. Vesely, C. K., Letiecq, B. L., & Goodman, R. D. (2017). Immigrant family resilience in context: using a community-based approach to build a new conceptual model. Journal of Family Theory & Review, 9(1), 93–110. https://doi.org/10.1111/jftr.12177
14. Sanders, J., Munford, R., & Liebenberg, L. (2017). Positive youth development practices and better outcomes for high risk youth. Child Abuse and Neglect, 69, 201–212. https://doi.org/10.1016/j.chiabu.2017.04.029
15. Craig, S. L., Austin, A., Alessi, E. J., Mcinroy, L., & Keane, G. (2017). Minority stress and HERoic coping among ethnoracial sexual minority girls: Intersections of resilience. Journal of Adolescent Research, 32(5), 614–641. https://doi.org/10.1177/0743558416653217
16. Parker, S. (2016). Impact of Positive Youth Development services on resilience among adjudicated girls. https://scholarworks.waldenu.edu/dissertations
17. Clonan-Roy, K., Jacobs, C. E., & Nakkula, M. J. (2016). Towards a model of Positive Youth Development specific to girls of color: Perspectives on development, resilience, and empowerment. Gender Issues, 33, 96–121. https://doi.org/10.1007/s12147-016-9156-7
Citation
Johnson JE, Gren LH, & Frost CJ (2021). Mental Health for Latina Youth: The Need for Tailored Resiliency Interventions. Utah Women’s Health Review. doi: 10.26054/0D-KVST-A0HE
Gender and Surgical Provider Role Differences in Opioid Prescribing Practices among Different Patient Populations
Abstract
Background: Patients living in rural communities and patients with a cancer diagnosis are two populations potentially overlooked in opioid prescribing clinical decision making that may relate to the amount of overprescribed opioids in the post-surgical environment. Provider gender, surgical role, attitudes and knowledge may affect prescribing practices for these at-risk populations, but little research has been conducted to date assessing the interplay between these different factors.
Methods: A 35-item questionnaire was administered to surgeons, residents/ fellows (trainees), and advanced practice clinicians (APCs). Frequency statistics compared differences in provider attitudes, perceptions, and practices by gender, role, age, and time in practice looking at patients in rural versus urban communities as well as cancer versus non-cancer patients.
Results: Female providers were more likely to worry about their cancer patients being addicted to opioids and more likely to e-prescribe to rural patients. Surgeons and trainees self-reported that they gave the same amount of opioids to rural patients as urban patients however APCs were more likely to have no change in their prescribing practices (p=0.02). APCs were more likely to agree that it is easy to e-prescribe (56%) than surgeons (41%) and trainees (35%), so rural patients do not need different consideration. Surgeons (50%) and trainees (50%) agreed compared to APCs (0%) that it is easier to give more opioids so a patient does not have to get refills if needed for pain (p=0.03). Compared to APCs (5%), 21% of surgeons and 45% of trainees acknowledged giving more opioid narcotics to patients with cancer than patients without a cancer diagnosis (p<0.001). APC’s were mostly female (69%).
Conclusions: While surgeons and trainees reported that they usually gave the same amount of opioids to rural patients, APCs were more likely to report that they didn’t change their practice based on a patient’s rural location, furthermore, providers differed in their knowledge about e-prescribing and what healthcare access disparities may exist for the rural patient. Surgeons and trainees were more likely than APCs to give more opioids to their cancer patients in comparison to their non-cancer patients. Responses indicate an opportunity to provide educational interventions with providers adapted to differences in gender and roles to identify potential solutions for improving opioid prescribing practices in rural verses urban and cancer verses non-cancer patients.
Introduction
Opioid overprescribing has been attributed as a major cause of the opioid epidemic currently facing society.1, 2 Prescribing providers’ behaviors contribute to overprescribing of opioid narcotics.3, 4 Knowledge of opioid prescribing guidelines and drug monitoring programs can help providers in clinical decision making regarding opioid prescribing for their patients.5 Therefore, understanding surgical providers’ prescribing behaviors and how they differ based on gender and their surgical role can lead to tailored interventions with the goal to reduce the amount of opioids that are overprescribed.
Differences in patient opioid use and gender are well documented as it relates to the opioid epidemic.6-8 However, while these issues have been described, gender differences related to opioid prescribing have not been adequately addressed, nor have interventions and programs related to reducing opioid prescribing at the provider level. 9, 10 Though female providers often represent a minority in the surgical setting11, their beliefs and practices can have a big impact on their patients.
Rural patients have also been shown to be at higher risk for opioid misuse due to socioeconomic factors and prior illicit drug use.12, 13 Rural occupations are often more physically demanding putting patients at higher risk for chronic pain and injuries since they often include mining and farming.14, 15 In fact, it has been estimated that patients living in rural areas are 20-30% more likely to fatally overdose on opioid narcotics than patients living in an urban setting partially due to demographic factors, but also because of difficulties in access to emergency care facilities and services.16 Prescribing providers have to balance the pain management needs of their patients living in rural areas and their access to care with the high potential for misuse.
Cancer patients are another population warranting additional considerations for post-surgical pain management, since their needs tend to involve both acute after surgery pain as well as chronic pain caused by their malignant condition.17, 18 It is estimated that 40-50% of cancer patients have moderate to severe pain during cancer treatment as well as after when they are in remission and beyond.19 The risk of new and persistent opioid use in opioid-naïve cancer patients is reported to be as high as 10.4%.19 With the potential for opioid dependence occurring in as little as days,20, 21 this unique combination of acute and chronic pain creates a maelstrom for cancer patients.
The aim of this study was to understand differences in gender and role between surgeons, trainees, and advanced practice clinicians (APCs) regarding post-surgical opioid prescribing to populations of rural verses urban and cancer verses non-cancer patients.
Methods
Study Design:
This was a descriptive, cross-sectional survey on provider opioid prescribing, we examined differences in providers’ opioid prescribing attitudes, perceptions, and practices regarding patients with cancer diagnoses and those living in rural areas. The study was a single-institution study within the University of Utah Health, Department of Surgery between July and September 2018. The study received approval from the University of Utah Institutional Review Board.
Survey:
An anonymous, 35-question instrument including demographic multiple choice and 5-point Likert scale items was developed by an expert committee. Questions were generated based upon anecdotal evidence of prescribing increases in rural and cancer populations and a review of the literature. The questionnaire was then iteratively pilot tested with four volunteer surgeons from multiple disciplines within the target population, who reviewed the questions for content applicability in April 2018. Changes were made based on feedback received and applied to the final questionnaire. During July through September 2018, an electronic link to the web-based REDCap22 questionnaire was provided to 242 providers (surgeons, residents/fellows (trainees), and advanced practice clinicians [APCs]) in nine disciplines at the University of Utah Health Department of Surgery. Participants were asked to self-identify their gender as male, female, or an open ended category that they could write in any gender identification.
Statistical Analysis:
Descriptive statistics were calculated on categorical variables. Univariate analyses were conducted using the chi-squared tests or Fisher’s exact test, as appropriate. The primary outcomes were self-reported practices of increased prescribing to patients with cancer or living in a rural location.
Likert scale questions were combined to show agreement (“agree” and “somewhat agree”) and disagreement, neutral was kept in a separate category due to low numbers in some categories. Frequency statistics compared differences in attitudes, perceptions, and practices by gender, role, age, and time in practice. The primary outcome variable was giving increased opioids to rural and cancer patients by surgical role. Prevalence ratios were generated using log-binomial models with surgeons as the reference group for dichotomous variables, with categorizing of variables into agreement and disagreement. 95% confidence intervals were also calculated. Covariates were adjusted on provider age and gender to account for differences in training and socially constructed roles and behaviors associated with gender. Data analysis was completed using Stata 15.1 software (College Station, TX).
Results
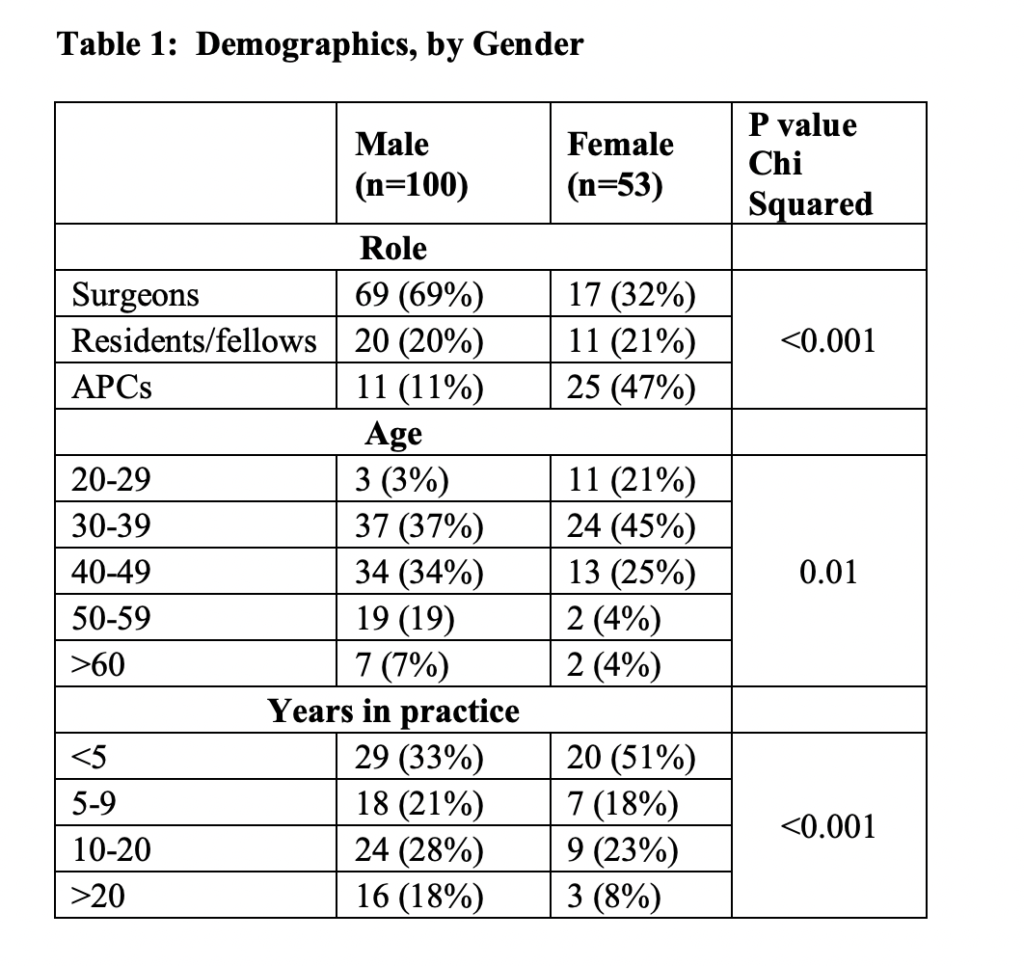
A total of 153/242 participants (64% response rate) responded to the questionnaire, with 86 (56%) surgeons, 31 (20%) trainees, and 36 (24%) APCs (Table 1). Females represented a minority at 33% of the total population, which is consistent with the target population demographics in the Department of Surgery, however, they had a 92% response rate. APC’s were mostly female (69%). The nine divisions within the Department of Surgery include: General Surgery, Transplant and Hepatobiliary Surgery, Emergency Medicine, Cardiothoracic Surgery, Vascular Surgery, Urology, Otolaryngology, Pediatric Surgery, and Plastic Surgery.
There was significant variation in role, age, and years in practice between men and women (with women tending to be APCs, younger, and have fewer years in practice) (p<0.001) (Table 1).
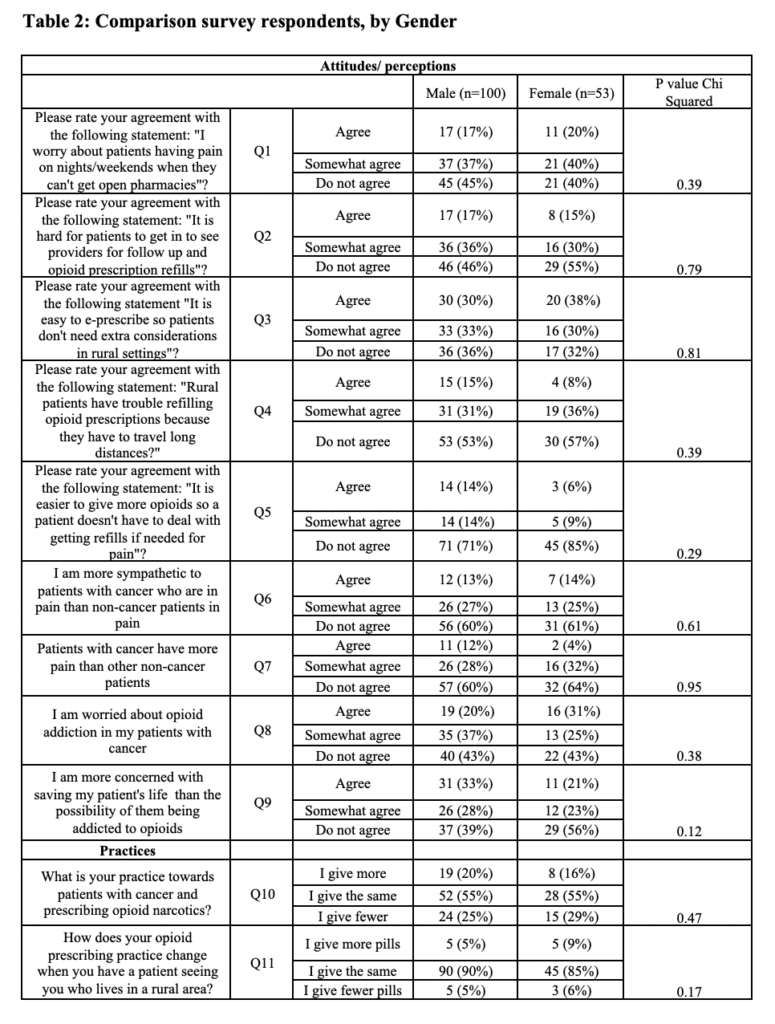
In unadjusted univariate analyses, females responded similarly to males in their agreement and/or disagreement in the categories looking at differences between rural and urban patients as well as in cancer versus non-cancer patients (Table 2).
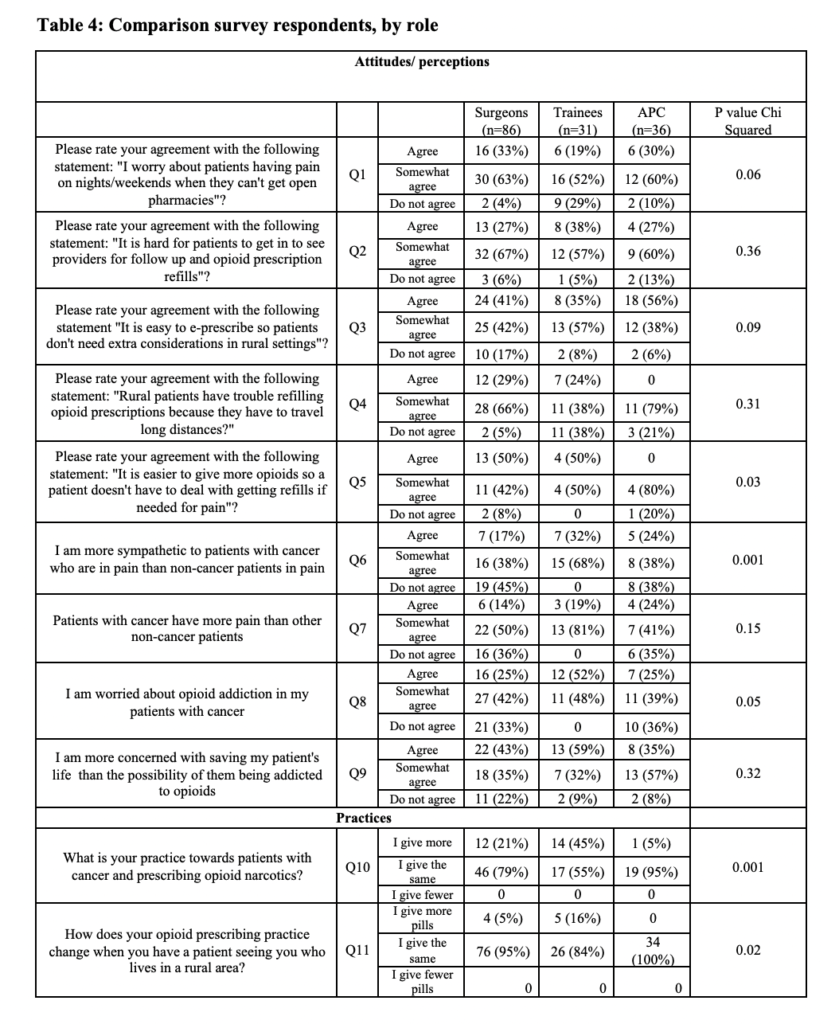
In contrast to separate questions, prescribing providers (surgeons [95%], trainees [84%], and APCs [100%]) self-reported that compared to urban patients, they give the same amount of opioids to rural patients. However, when questioned further, trainees acknowledged being more likely to give more opioids to rural patients (surgeon versus trainee, adjusted prevalence ratios (aPR)= 3.9, 95% CI 1.4-38.0) (p=0.02) (Table 3). Surgeons (96%), trainees (71%) and APCs (90%) all agreed or somewhat agreed that they worry about rural patients having pain with no open pharmacies on nights and weekends (p=0.06). APCs were more likely to agree that it is easy to e-prescribe (56%) than physicians (41%) or trainees (35%), so rural patients do not need different consideration (p=0.09) (Table 4). Surgeons (29%) and trainees (24%) were more likely to agree that rural patients have trouble refilling opioid prescriptions because they have to travel long distances than APCs (0%) (p=0.31). Surgeons (50%) and trainees (50%) agreed, relative to APCs (0%), that it is easier to give more opioids so a patient does not have to acquire refills if needed for pain (p=0.03). All groups of providers agreed that it is hard for patients to get in to see providers for opioid refills (p=0.36) (Table 4).
When asked about their practice, 5% of APCs compared to 21% of surgeons and 45% of trainees acknowledged giving more opioid narcotics to patients with cancer than non-cancer patients (p<0.001). Trainees were more likely to report giving more opioids in their practice to cancer patients than APCs or surgeons when accounting for age and gender (surgeon versus trainee aPR=22.14, 95% CI 1.8-28.1) (Table 3).
Providers reported that they either agree or somewhat agree that they are more sympathetic to patients with cancer versus non-cancer patients, surgeons (54%), trainees (100%), and APCs (62%) (p<0.001). Trainees (100%) reported at a higher percentage than either surgeons (64%) or APCs (64%) that cancer patients have the same amount of pain as non-cancer patients (p=0.15). Surgeons (67%), trainees (100%), and APCs (64%) either agreed or somewhat agreed that they are worried about opioid addiction in their patients with cancer (p=0.05). Trainees (59%) and surgeons (43%) appeared more likely than APCs (35%) to acknowledge that they were more concerned about saving their patient’s life than the possibility that they could become addicted to opioids (p=0.32) (Table 3).

Discussion
The current study investigates surgical provider perceptions and beliefs about patients with cancer versus non-cancer and patients living in rural versus non-rural areas regarding pain management according to their role and gender.
While there were relatively few differences in agreement regarding patients and opioid prescribing factors according to gender, a more likely explanation is that APCs are more likely to be female (69%) which is impacting prescribing.
We found that APCs’ opioid prescribing practices were less influenced than surgeons or trainees on the rural location of their patients. However, their knowledge and beliefs regarding potential disparities in access to care and pain management faced by rural patients were different by provider type. Half of surgeons and trainees answered that it is easier for them to give more opioids so a patient does not have to acquire refills when compared to APCs (p=0.03). Surgeons, trainees, and APCs also answered that their patients do indeed have difficulty getting in to see them for refills due to long distances (p=0.36). These attitudes and beliefs could potentially impact actual prescribing practices by either overprescribing opioids or the reverse by not meeting patient needs. This is similar to previously reported literature that showed rural patients were more likely to have an opioid prescription than similar cohorts in urban areas.12
While surgeons, trainees, and APCs agreed that cancer patients have the same rates of postoperative pain as their other patients, surgeons and trainees more frequently acknowledged giving more opioid narcotics to patients with cancer in this study. While cancer patients in general have both acute and chronic pain due to their underlying diagnosis and subsequent sequelae, from a surgical perspective, the respondents were in line with what is generally accepted that the surgical pain should be the same regardless of cancer morbidity.18 However, in 2017, Deshields et al. performed a large study with 301 non-cancer patients (NCP) and 558 cancer patients (CP) and found that NCPs had a higher reported rate of pain when compared to CPs (45% of CP versus 54% of NCP).23 This finding could be due to a higher tolerance for pain from the cancer patient group due to having higher baseline pain due to chronic conditions.23
This contrast in practice and belief may represent an area for improvement and advocacy and warrants further study to determine if underlying bias or sympathy for cancer patients is affecting actual prescribing practices.19 This is similar to other studies that found that cancer patients were more likely to have an opioid prescription than a non-cancer patient and that they are at high risk for opioid misuse.17-19
Throughout the study, trainees reported similarly in their responses to surgeons when compared to APCs. The structure of resident and fellow training by shadowing and learning under the close supervision of surgeons in an academic medical center24 would intrinsically be expected to foster similarities between the two groups. While APCs also receive supervision from the surgeons, their attitudes and perceptions differed more frequently from them then did the trainees. This could also argue that the initial medical education from either medical school for residents and fellows or nurse practitioner and physician assistant school has an important role in facilitating attitudes and perceptions regarding opioid prescribing. In many surgical practices, APCs have taken over the day-to-day management of patients and may therefore be more likely to perceive the importance of pain management for patients. This finding may also tie into the fact that APCs are spending more individual time with the patient due to surgeon time limitations.
The major limitation of our study is that it was done at a single institution. Homogeneity of the institutional culture and commonalities in the health system may limit the generalizability of our findings. We do not anticipate that this single institution was intrinsically different than other institutions. Furthermore, though we had a 92% response rate among female providers, it is still a small sample size. Another limitation is that the survey depended on self-reporting. We were not able to compare provider responses with their actual prescribing practices as the surveys were anonymous to encourage responses. It is possible that providers may be over-estimating their awareness and application of guidelines or other practices they view as socially desirable. Healthcare workers may conform to rules of an institution despite their personal values.25 However, we attempted to reduce this bias by keeping survey responses anonymous. Furthermore, it is possible that the response rate was substantially higher among those providers who view overprescribing as a serious problem. Other methods such as qualitative interviews or focus groups may be helpful in identifying potential barriers to improvement.
Conclusion
APCs more frequently reported that they gave the same amount of opioids to rural patients that they give to urban patients. However, prescribing providers differed in their attitudes and perceptions about e-prescribing and potential disparities that exist for the rural patient by gender and surgical role. This was also the case for cancer patients in that surgeons gave more opioids to cancer patients despite not reporting that they thought cancer patients have more pain than others. Therefore, in regards to rural and cancer patients and potential disparities, there seems to be an opportunity for improvement and educational interventions based on gender and the role of prescribing providers. This could include more systematic guidelines and identification of rural and cancer populations built into the care pathways can lead to individual level discussion in order to evaluate possible barriers and mitigate risk for these patients.
Abbreviations
APC— Advanced practice clinicians
CP— Cancer patients
NCP— Non-cancer patients
Declarations
Ethics Approval and Consent to Participate: This study was approved in accordance with the guidelines and principles of the University of Utah Institutional Review Board and a consent cover letter was utilized. As this was an anonymous survey, documentation of informed consent was not obtained per IRB requirements and approval. It was implied that those who continued with the survey after the consent cover letter gave consent for participation.
Availability of Data and Material: Data and material are available upon request.
Competing Interests: There are no competing interests associated with the research presented herein.
Funding: REDCap support provided by UL1TR002538 NCATS/NIH.
Authors’ Contributions: HT, LH, VV, LG, CP crafted the research question, hypothesis, and study design. HT and LH created the survey. HT, LH, VV, LG, and CP collected the data. HT performed the data analysis while LH, VV, LG, and CP provided critical interpretation of the data. HT drafted the manuscript. LH, VV, LG, and CP provided essential revisions to the manuscript. All authors have read and approved the manuscript.
References
1. Makary Ma Fau – Overton HN, Overton Hn Fau – Wang P, Wang P. Overprescribing is major contributor to opioid crisis. (1756-1833 (Electronic)).
2. Clark DJ, Schumacher MA. America’s Opioid Epidemic: Supply and Demand Considerations. (1526-7598 (Electronic)).
3. Cheatle MD. The Impact of Prescription Drug Monitoring Programs and Prescribing Guidelines on Opioid Prescribing Behaviors: A Time for Institutional and Regulatory Changes. (1526-4637 (Electronic)).
4. Pomerleau AC, Nelson LS, Hoppe JA, Salzman M, Weiss PS, Perrone J. The Impact of Prescription Drug Monitoring Programs and Prescribing Guidelines on Emergency Department Opioid Prescribing: A Multi-Center Survey. (1526-4637 (Electronic)).
5. Leichtling GJ, Irvine JM, Hildebran C, Cohen DJ, Hallvik SE, Deyo RA. Clinicians’ Use of Prescription Drug Monitoring Programs in Clinical Practice and Decision-Making. (1526-4637 (Electronic)).
6. Serdarevic M, Striley CW, Gurka KK, Leeman RF, LB C. Sex differences in prescription opioid use patterns assessed through a community engagement program in Florida. Drug Alcohol Dependence. 2019;204(107568).
7. Serdarevic M, Striley CW, Cottler LB. Sex differences in prescription opioid use. Current opinion in psychiatry. 2017;30(4):238-246.
8. Green TC, Grimes Serrano JM, Licari A, Budman SH, Butler SF. Women who abuse prescription opioids: findings from the Addiction Severity Index-Multimedia Version Connect prescription opioid database. Drug and alcohol dependence. 2009;103(1-2):65-73.
9. Jena AB, Goldman D, Weaver L, Karaca-Mandic P. Opioid prescribing by multiple providers in Medicare: retrospective observational study of insurance claims. BMJ (Clinical research ed.). 2014;348:g1393-g1393.
10. Klueh MP, Sloss KR, Dossett LA, et al. Postoperative opioid prescribing is not my job: A qualitative analysis of care transitions. Surgery. 2019;166(5):744-751.
11. Yu PTP, P. V.; Hassanein, O.; Rogers, S. O.; Chang, D. C. Minorities struggle to advance in academic medicine: A 12-y review of diversity at the highest levels of America’s teaching institutions. The Journal of Surgical Research. 2013;182(2):212–218.
12. Cochran GT, Engel RJ, Hruschak VJ, Tarter RE. Prescription Opioid Misuse Among Rural Community Pharmacy Patients: Pilot Study for Screening and Implications for Future Practice and Research. (1531-1937 (Electronic)).
13. Monnat SM, Rigg KK. Examining Rural/Urban Differences in Prescription Opioid Misuse Among US Adolescents. (1748-0361 (Electronic)).
14. Eaton LH, Langford DJ, Meins AR, Rue T, Tauben DJ, Doorenbos AZ. Use of Self-management Interventions for Chronic Pain Management: A Comparison between Rural and Nonrural Residents. Pain management nursing : official journal of the American Society of Pain Management Nurses. 2018;19(1):8-13.
15. Hoffman PK MB, Council JR. A comparison of chronic pain between an urban and rural population. J Community Health Nurs. 2002;19(4):213-224.
16. Mosher H, Zhou Y, Thurman AL, Sarrazin MV, Ohl ME. Trends in Hospitalization for Opioid Overdose among Rural Compared to Urban Residents of the United States, 2007-2014. (1553-5606 (Electronic)).
17. Liang Y, Bao G, Gong L, et al. Evaluating the analgesic effect and advantage of transcutaneous electrical acupoint stimulation combined with opioid drugs for moderate to severe cancer-related pain: a study protocol for a randomized controlled trial. (1745-6215 (Electronic)).
18. Fradkin M, Batash R, Elamleh S, et al. Management of peripheral neuropathy induced by chemotherapy. LID – 10.2174/0929867326666190107163756 [doi]. (1875-533X (Electronic)).
19. Bennett M, Paice JA, Wallace M. Pain and Opioids in Cancer Care: Benefits, Risks, and Alternatives. (1548-8756 (Electronic)).
20. Kosten TR, George TP. The neurobiology of opioid dependence: implications for treatment. Science & practice perspectives. 2002;1(1):13-20.
21. Prevention USCfDCa. Opioid Dependence Can Start in Just a Few Days. Morbidity and Mortality Weekly Report. March 17 2017.
22. Harris PA, Taylor R Fau – Thielke R, Thielke R Fau – Payne J, Payne J Fau – Gonzalez N, Gonzalez N Fau – Conde JG, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. (1532-0480 (Electronic)).
23. Deshields TL, Penalba V, Liu J, Avery J. Comparing the symptom experience of cancer patients and non-cancer patients. (1433-7339 (Electronic)).
24. Surgery D. Residencies and Fellowships. Available at: https://medicine.utah.edu/surgery/residencies-fellowships.php. Accessed March 26, 2019.
25. Hermann H, Trachsel M, Biller-Andorno N. Physicians’ personal values in determining medical decision-making capacity: a survey study. (1473-4257 (Electronic)).
Citation
Thiesset HF, Huang LC, Valentin VL, Gren LH, & Porucznik CA. (2021). Gender and Surgical Provider Role Differences in Opioid Prescribing Practices among Different Patient Populations. Utah Women’s Health Review. doi: 10.26054/0D-N2BB-H2GC

