Table of Contents
Abstract
Background: Patients living in rural communities and patients with a cancer diagnosis are two populations potentially overlooked in opioid prescribing clinical decision making that may relate to the amount of overprescribed opioids in the post-surgical environment. Provider gender, surgical role, attitudes and knowledge may affect prescribing practices for these at-risk populations, but little research has been conducted to date assessing the interplay between these different factors.
Methods: A 35-item questionnaire was administered to surgeons, residents/ fellows (trainees), and advanced practice clinicians (APCs). Frequency statistics compared differences in provider attitudes, perceptions, and practices by gender, role, age, and time in practice looking at patients in rural versus urban communities as well as cancer versus non-cancer patients.
Results: Female providers were more likely to worry about their cancer patients being addicted to opioids and more likely to e-prescribe to rural patients. Surgeons and trainees self-reported that they gave the same amount of opioids to rural patients as urban patients however APCs were more likely to have no change in their prescribing practices (p=0.02). APCs were more likely to agree that it is easy to e-prescribe (56%) than surgeons (41%) and trainees (35%), so rural patients do not need different consideration. Surgeons (50%) and trainees (50%) agreed compared to APCs (0%) that it is easier to give more opioids so a patient does not have to get refills if needed for pain (p=0.03). Compared to APCs (5%), 21% of surgeons and 45% of trainees acknowledged giving more opioid narcotics to patients with cancer than patients without a cancer diagnosis (p<0.001). APC’s were mostly female (69%).
Conclusions: While surgeons and trainees reported that they usually gave the same amount of opioids to rural patients, APCs were more likely to report that they didn’t change their practice based on a patient’s rural location, furthermore, providers differed in their knowledge about e-prescribing and what healthcare access disparities may exist for the rural patient. Surgeons and trainees were more likely than APCs to give more opioids to their cancer patients in comparison to their non-cancer patients. Responses indicate an opportunity to provide educational interventions with providers adapted to differences in gender and roles to identify potential solutions for improving opioid prescribing practices in rural verses urban and cancer verses non-cancer patients.
Introduction
Opioid overprescribing has been attributed as a major cause of the opioid epidemic currently facing society.1, 2 Prescribing providers’ behaviors contribute to overprescribing of opioid narcotics.3, 4 Knowledge of opioid prescribing guidelines and drug monitoring programs can help providers in clinical decision making regarding opioid prescribing for their patients.5 Therefore, understanding surgical providers’ prescribing behaviors and how they differ based on gender and their surgical role can lead to tailored interventions with the goal to reduce the amount of opioids that are overprescribed.
Differences in patient opioid use and gender are well documented as it relates to the opioid epidemic.6-8 However, while these issues have been described, gender differences related to opioid prescribing have not been adequately addressed, nor have interventions and programs related to reducing opioid prescribing at the provider level. 9, 10 Though female providers often represent a minority in the surgical setting11, their beliefs and practices can have a big impact on their patients.
Rural patients have also been shown to be at higher risk for opioid misuse due to socioeconomic factors and prior illicit drug use.12, 13 Rural occupations are often more physically demanding putting patients at higher risk for chronic pain and injuries since they often include mining and farming.14, 15 In fact, it has been estimated that patients living in rural areas are 20-30% more likely to fatally overdose on opioid narcotics than patients living in an urban setting partially due to demographic factors, but also because of difficulties in access to emergency care facilities and services.16 Prescribing providers have to balance the pain management needs of their patients living in rural areas and their access to care with the high potential for misuse.
Cancer patients are another population warranting additional considerations for post-surgical pain management, since their needs tend to involve both acute after surgery pain as well as chronic pain caused by their malignant condition.17, 18 It is estimated that 40-50% of cancer patients have moderate to severe pain during cancer treatment as well as after when they are in remission and beyond.19 The risk of new and persistent opioid use in opioid-naïve cancer patients is reported to be as high as 10.4%.19 With the potential for opioid dependence occurring in as little as days,20, 21 this unique combination of acute and chronic pain creates a maelstrom for cancer patients.
The aim of this study was to understand differences in gender and role between surgeons, trainees, and advanced practice clinicians (APCs) regarding post-surgical opioid prescribing to populations of rural verses urban and cancer verses non-cancer patients.
Methods
Study Design:
This was a descriptive, cross-sectional survey on provider opioid prescribing, we examined differences in providers’ opioid prescribing attitudes, perceptions, and practices regarding patients with cancer diagnoses and those living in rural areas. The study was a single-institution study within the University of Utah Health, Department of Surgery between July and September 2018. The study received approval from the University of Utah Institutional Review Board.
Survey:
An anonymous, 35-question instrument including demographic multiple choice and 5-point Likert scale items was developed by an expert committee. Questions were generated based upon anecdotal evidence of prescribing increases in rural and cancer populations and a review of the literature. The questionnaire was then iteratively pilot tested with four volunteer surgeons from multiple disciplines within the target population, who reviewed the questions for content applicability in April 2018. Changes were made based on feedback received and applied to the final questionnaire. During July through September 2018, an electronic link to the web-based REDCap22 questionnaire was provided to 242 providers (surgeons, residents/fellows (trainees), and advanced practice clinicians [APCs]) in nine disciplines at the University of Utah Health Department of Surgery. Participants were asked to self-identify their gender as male, female, or an open ended category that they could write in any gender identification.
Statistical Analysis:
Descriptive statistics were calculated on categorical variables. Univariate analyses were conducted using the chi-squared tests or Fisher’s exact test, as appropriate. The primary outcomes were self-reported practices of increased prescribing to patients with cancer or living in a rural location.
Likert scale questions were combined to show agreement (“agree” and “somewhat agree”) and disagreement, neutral was kept in a separate category due to low numbers in some categories. Frequency statistics compared differences in attitudes, perceptions, and practices by gender, role, age, and time in practice. The primary outcome variable was giving increased opioids to rural and cancer patients by surgical role. Prevalence ratios were generated using log-binomial models with surgeons as the reference group for dichotomous variables, with categorizing of variables into agreement and disagreement. 95% confidence intervals were also calculated. Covariates were adjusted on provider age and gender to account for differences in training and socially constructed roles and behaviors associated with gender. Data analysis was completed using Stata 15.1 software (College Station, TX).
Results
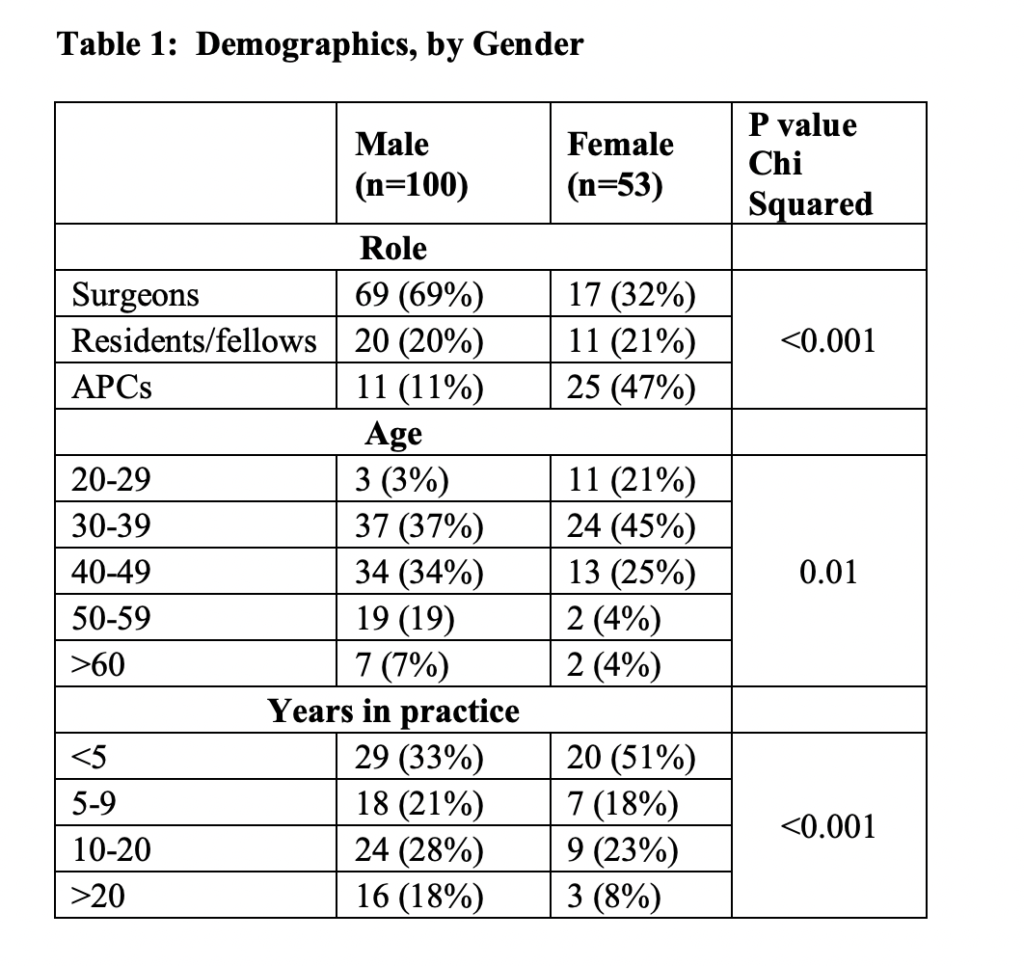
A total of 153/242 participants (64% response rate) responded to the questionnaire, with 86 (56%) surgeons, 31 (20%) trainees, and 36 (24%) APCs (Table 1). Females represented a minority at 33% of the total population, which is consistent with the target population demographics in the Department of Surgery, however, they had a 92% response rate. APC’s were mostly female (69%). The nine divisions within the Department of Surgery include: General Surgery, Transplant and Hepatobiliary Surgery, Emergency Medicine, Cardiothoracic Surgery, Vascular Surgery, Urology, Otolaryngology, Pediatric Surgery, and Plastic Surgery.
There was significant variation in role, age, and years in practice between men and women (with women tending to be APCs, younger, and have fewer years in practice) (p<0.001) (Table 1).
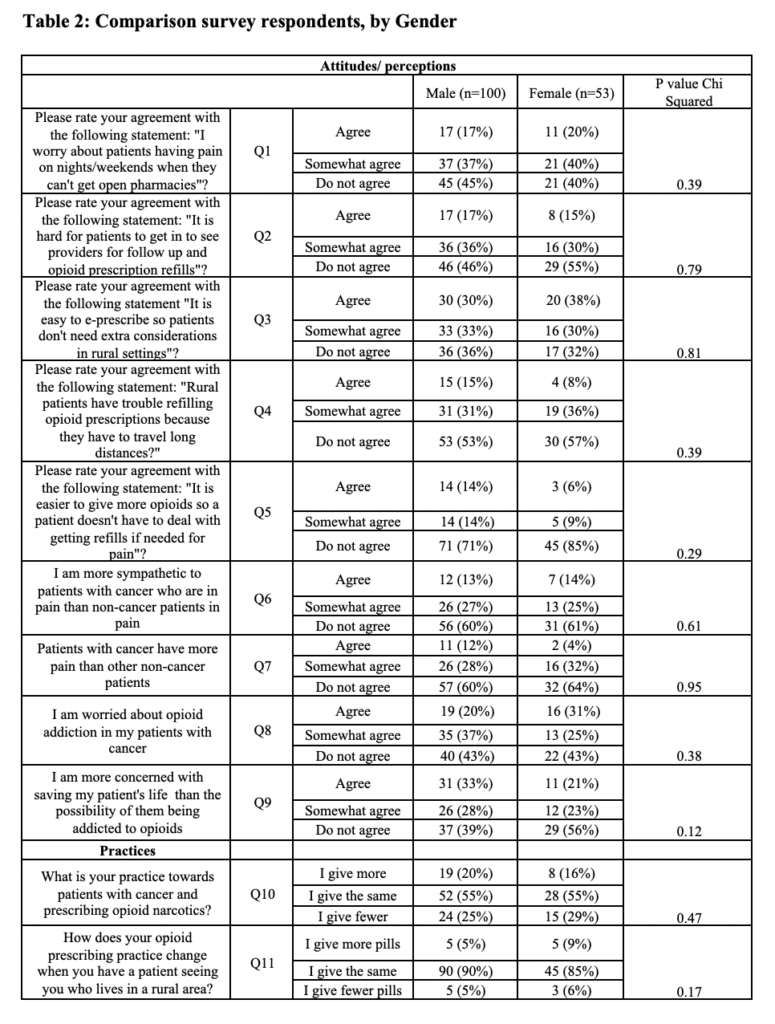
In unadjusted univariate analyses, females responded similarly to males in their agreement and/or disagreement in the categories looking at differences between rural and urban patients as well as in cancer versus non-cancer patients (Table 2).
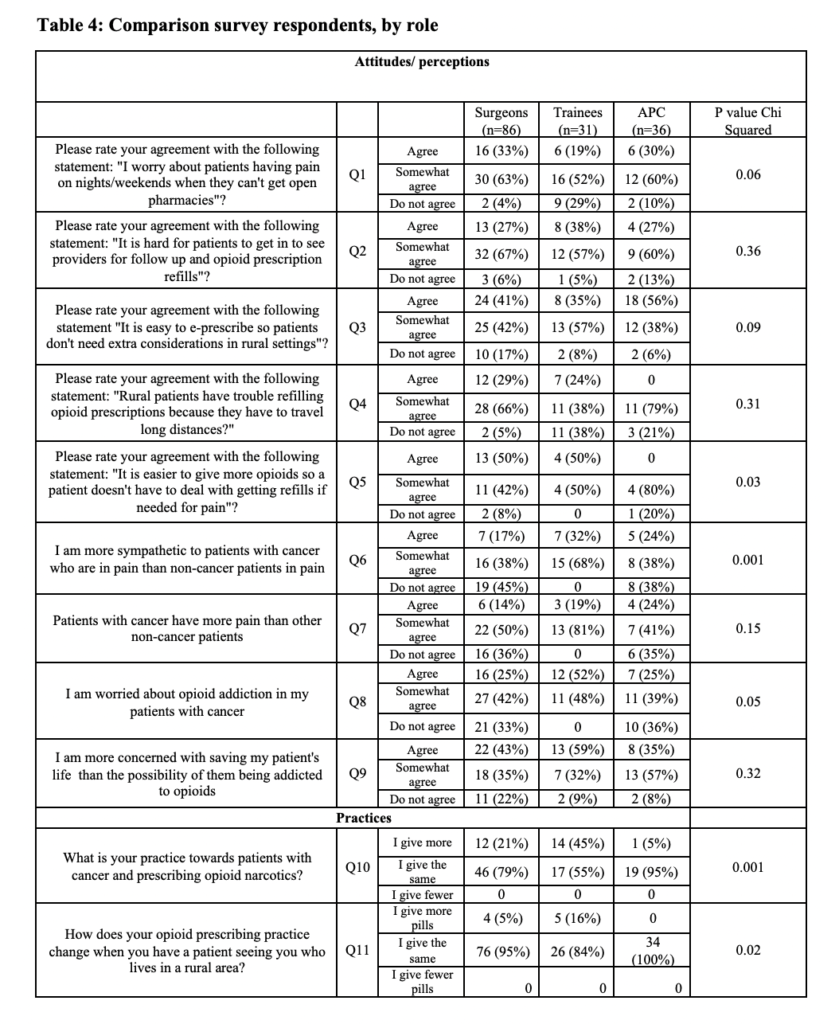
In contrast to separate questions, prescribing providers (surgeons [95%], trainees [84%], and APCs [100%]) self-reported that compared to urban patients, they give the same amount of opioids to rural patients. However, when questioned further, trainees acknowledged being more likely to give more opioids to rural patients (surgeon versus trainee, adjusted prevalence ratios (aPR)= 3.9, 95% CI 1.4-38.0) (p=0.02) (Table 3). Surgeons (96%), trainees (71%) and APCs (90%) all agreed or somewhat agreed that they worry about rural patients having pain with no open pharmacies on nights and weekends (p=0.06). APCs were more likely to agree that it is easy to e-prescribe (56%) than physicians (41%) or trainees (35%), so rural patients do not need different consideration (p=0.09) (Table 4). Surgeons (29%) and trainees (24%) were more likely to agree that rural patients have trouble refilling opioid prescriptions because they have to travel long distances than APCs (0%) (p=0.31). Surgeons (50%) and trainees (50%) agreed, relative to APCs (0%), that it is easier to give more opioids so a patient does not have to acquire refills if needed for pain (p=0.03). All groups of providers agreed that it is hard for patients to get in to see providers for opioid refills (p=0.36) (Table 4).
When asked about their practice, 5% of APCs compared to 21% of surgeons and 45% of trainees acknowledged giving more opioid narcotics to patients with cancer than non-cancer patients (p<0.001). Trainees were more likely to report giving more opioids in their practice to cancer patients than APCs or surgeons when accounting for age and gender (surgeon versus trainee aPR=22.14, 95% CI 1.8-28.1) (Table 3).
Providers reported that they either agree or somewhat agree that they are more sympathetic to patients with cancer versus non-cancer patients, surgeons (54%), trainees (100%), and APCs (62%) (p<0.001). Trainees (100%) reported at a higher percentage than either surgeons (64%) or APCs (64%) that cancer patients have the same amount of pain as non-cancer patients (p=0.15). Surgeons (67%), trainees (100%), and APCs (64%) either agreed or somewhat agreed that they are worried about opioid addiction in their patients with cancer (p=0.05). Trainees (59%) and surgeons (43%) appeared more likely than APCs (35%) to acknowledge that they were more concerned about saving their patient’s life than the possibility that they could become addicted to opioids (p=0.32) (Table 3).

Discussion
The current study investigates surgical provider perceptions and beliefs about patients with cancer versus non-cancer and patients living in rural versus non-rural areas regarding pain management according to their role and gender.
While there were relatively few differences in agreement regarding patients and opioid prescribing factors according to gender, a more likely explanation is that APCs are more likely to be female (69%) which is impacting prescribing.
We found that APCs’ opioid prescribing practices were less influenced than surgeons or trainees on the rural location of their patients. However, their knowledge and beliefs regarding potential disparities in access to care and pain management faced by rural patients were different by provider type. Half of surgeons and trainees answered that it is easier for them to give more opioids so a patient does not have to acquire refills when compared to APCs (p=0.03). Surgeons, trainees, and APCs also answered that their patients do indeed have difficulty getting in to see them for refills due to long distances (p=0.36). These attitudes and beliefs could potentially impact actual prescribing practices by either overprescribing opioids or the reverse by not meeting patient needs. This is similar to previously reported literature that showed rural patients were more likely to have an opioid prescription than similar cohorts in urban areas.12
While surgeons, trainees, and APCs agreed that cancer patients have the same rates of postoperative pain as their other patients, surgeons and trainees more frequently acknowledged giving more opioid narcotics to patients with cancer in this study. While cancer patients in general have both acute and chronic pain due to their underlying diagnosis and subsequent sequelae, from a surgical perspective, the respondents were in line with what is generally accepted that the surgical pain should be the same regardless of cancer morbidity.18 However, in 2017, Deshields et al. performed a large study with 301 non-cancer patients (NCP) and 558 cancer patients (CP) and found that NCPs had a higher reported rate of pain when compared to CPs (45% of CP versus 54% of NCP).23 This finding could be due to a higher tolerance for pain from the cancer patient group due to having higher baseline pain due to chronic conditions.23
This contrast in practice and belief may represent an area for improvement and advocacy and warrants further study to determine if underlying bias or sympathy for cancer patients is affecting actual prescribing practices.19 This is similar to other studies that found that cancer patients were more likely to have an opioid prescription than a non-cancer patient and that they are at high risk for opioid misuse.17-19
Throughout the study, trainees reported similarly in their responses to surgeons when compared to APCs. The structure of resident and fellow training by shadowing and learning under the close supervision of surgeons in an academic medical center24 would intrinsically be expected to foster similarities between the two groups. While APCs also receive supervision from the surgeons, their attitudes and perceptions differed more frequently from them then did the trainees. This could also argue that the initial medical education from either medical school for residents and fellows or nurse practitioner and physician assistant school has an important role in facilitating attitudes and perceptions regarding opioid prescribing. In many surgical practices, APCs have taken over the day-to-day management of patients and may therefore be more likely to perceive the importance of pain management for patients. This finding may also tie into the fact that APCs are spending more individual time with the patient due to surgeon time limitations.
The major limitation of our study is that it was done at a single institution. Homogeneity of the institutional culture and commonalities in the health system may limit the generalizability of our findings. We do not anticipate that this single institution was intrinsically different than other institutions. Furthermore, though we had a 92% response rate among female providers, it is still a small sample size. Another limitation is that the survey depended on self-reporting. We were not able to compare provider responses with their actual prescribing practices as the surveys were anonymous to encourage responses. It is possible that providers may be over-estimating their awareness and application of guidelines or other practices they view as socially desirable. Healthcare workers may conform to rules of an institution despite their personal values.25 However, we attempted to reduce this bias by keeping survey responses anonymous. Furthermore, it is possible that the response rate was substantially higher among those providers who view overprescribing as a serious problem. Other methods such as qualitative interviews or focus groups may be helpful in identifying potential barriers to improvement.
Conclusion
APCs more frequently reported that they gave the same amount of opioids to rural patients that they give to urban patients. However, prescribing providers differed in their attitudes and perceptions about e-prescribing and potential disparities that exist for the rural patient by gender and surgical role. This was also the case for cancer patients in that surgeons gave more opioids to cancer patients despite not reporting that they thought cancer patients have more pain than others. Therefore, in regards to rural and cancer patients and potential disparities, there seems to be an opportunity for improvement and educational interventions based on gender and the role of prescribing providers. This could include more systematic guidelines and identification of rural and cancer populations built into the care pathways can lead to individual level discussion in order to evaluate possible barriers and mitigate risk for these patients.
Abbreviations
APC— Advanced practice clinicians
CP— Cancer patients
NCP— Non-cancer patients
Declarations
Ethics Approval and Consent to Participate: This study was approved in accordance with the guidelines and principles of the University of Utah Institutional Review Board and a consent cover letter was utilized. As this was an anonymous survey, documentation of informed consent was not obtained per IRB requirements and approval. It was implied that those who continued with the survey after the consent cover letter gave consent for participation.
Availability of Data and Material: Data and material are available upon request.
Competing Interests: There are no competing interests associated with the research presented herein.
Funding: REDCap support provided by UL1TR002538 NCATS/NIH.
Authors’ Contributions: HT, LH, VV, LG, CP crafted the research question, hypothesis, and study design. HT and LH created the survey. HT, LH, VV, LG, and CP collected the data. HT performed the data analysis while LH, VV, LG, and CP provided critical interpretation of the data. HT drafted the manuscript. LH, VV, LG, and CP provided essential revisions to the manuscript. All authors have read and approved the manuscript.
References
1. Makary Ma Fau – Overton HN, Overton Hn Fau – Wang P, Wang P. Overprescribing is major contributor to opioid crisis. (1756-1833 (Electronic)).
2. Clark DJ, Schumacher MA. America’s Opioid Epidemic: Supply and Demand Considerations. (1526-7598 (Electronic)).
3. Cheatle MD. The Impact of Prescription Drug Monitoring Programs and Prescribing Guidelines on Opioid Prescribing Behaviors: A Time for Institutional and Regulatory Changes. (1526-4637 (Electronic)).
4. Pomerleau AC, Nelson LS, Hoppe JA, Salzman M, Weiss PS, Perrone J. The Impact of Prescription Drug Monitoring Programs and Prescribing Guidelines on Emergency Department Opioid Prescribing: A Multi-Center Survey. (1526-4637 (Electronic)).
5. Leichtling GJ, Irvine JM, Hildebran C, Cohen DJ, Hallvik SE, Deyo RA. Clinicians’ Use of Prescription Drug Monitoring Programs in Clinical Practice and Decision-Making. (1526-4637 (Electronic)).
6. Serdarevic M, Striley CW, Gurka KK, Leeman RF, LB C. Sex differences in prescription opioid use patterns assessed through a community engagement program in Florida. Drug Alcohol Dependence. 2019;204(107568).
7. Serdarevic M, Striley CW, Cottler LB. Sex differences in prescription opioid use. Current opinion in psychiatry. 2017;30(4):238-246.
8. Green TC, Grimes Serrano JM, Licari A, Budman SH, Butler SF. Women who abuse prescription opioids: findings from the Addiction Severity Index-Multimedia Version Connect prescription opioid database. Drug and alcohol dependence. 2009;103(1-2):65-73.
9. Jena AB, Goldman D, Weaver L, Karaca-Mandic P. Opioid prescribing by multiple providers in Medicare: retrospective observational study of insurance claims. BMJ (Clinical research ed.). 2014;348:g1393-g1393.
10. Klueh MP, Sloss KR, Dossett LA, et al. Postoperative opioid prescribing is not my job: A qualitative analysis of care transitions. Surgery. 2019;166(5):744-751.
11. Yu PTP, P. V.; Hassanein, O.; Rogers, S. O.; Chang, D. C. Minorities struggle to advance in academic medicine: A 12-y review of diversity at the highest levels of America’s teaching institutions. The Journal of Surgical Research. 2013;182(2):212–218.
12. Cochran GT, Engel RJ, Hruschak VJ, Tarter RE. Prescription Opioid Misuse Among Rural Community Pharmacy Patients: Pilot Study for Screening and Implications for Future Practice and Research. (1531-1937 (Electronic)).
13. Monnat SM, Rigg KK. Examining Rural/Urban Differences in Prescription Opioid Misuse Among US Adolescents. (1748-0361 (Electronic)).
14. Eaton LH, Langford DJ, Meins AR, Rue T, Tauben DJ, Doorenbos AZ. Use of Self-management Interventions for Chronic Pain Management: A Comparison between Rural and Nonrural Residents. Pain management nursing : official journal of the American Society of Pain Management Nurses. 2018;19(1):8-13.
15. Hoffman PK MB, Council JR. A comparison of chronic pain between an urban and rural population. J Community Health Nurs. 2002;19(4):213-224.
16. Mosher H, Zhou Y, Thurman AL, Sarrazin MV, Ohl ME. Trends in Hospitalization for Opioid Overdose among Rural Compared to Urban Residents of the United States, 2007-2014. (1553-5606 (Electronic)).
17. Liang Y, Bao G, Gong L, et al. Evaluating the analgesic effect and advantage of transcutaneous electrical acupoint stimulation combined with opioid drugs for moderate to severe cancer-related pain: a study protocol for a randomized controlled trial. (1745-6215 (Electronic)).
18. Fradkin M, Batash R, Elamleh S, et al. Management of peripheral neuropathy induced by chemotherapy. LID – 10.2174/0929867326666190107163756 [doi]. (1875-533X (Electronic)).
19. Bennett M, Paice JA, Wallace M. Pain and Opioids in Cancer Care: Benefits, Risks, and Alternatives. (1548-8756 (Electronic)).
20. Kosten TR, George TP. The neurobiology of opioid dependence: implications for treatment. Science & practice perspectives. 2002;1(1):13-20.
21. Prevention USCfDCa. Opioid Dependence Can Start in Just a Few Days. Morbidity and Mortality Weekly Report. March 17 2017.
22. Harris PA, Taylor R Fau – Thielke R, Thielke R Fau – Payne J, Payne J Fau – Gonzalez N, Gonzalez N Fau – Conde JG, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. (1532-0480 (Electronic)).
23. Deshields TL, Penalba V, Liu J, Avery J. Comparing the symptom experience of cancer patients and non-cancer patients. (1433-7339 (Electronic)).
24. Surgery D. Residencies and Fellowships. Available at: https://medicine.utah.edu/surgery/residencies-fellowships.php. Accessed March 26, 2019.
25. Hermann H, Trachsel M, Biller-Andorno N. Physicians’ personal values in determining medical decision-making capacity: a survey study. (1473-4257 (Electronic)).
Citation
Thiesset HF, Huang LC, Valentin VL, Gren LH, & Porucznik CA. (2021). Gender and Surgical Provider Role Differences in Opioid Prescribing Practices among Different Patient Populations. Utah Women’s Health Review. doi: 10.26054/0D-N2BB-H2GC

