Background
Although the infant mortality rate in the US appeared stagnant in the early 2000s, there has been a steady decrease in the overall rate since the 1990s.1 Compared to the national trend, infant mortality in Utah has not shown a striking decrease within the same time frame but has maintained a relatively steady slope downward.2-3 It has been determined that the leading causes of infant mortality in Utah are preterm birth, birth defects, sudden unexpected infant death (SUID), and medical conditions an infant may have that predisposes them to a shortened lifespan.2
Infant mortality is defined as the number of deaths in children under one year of age per 1000 live births in the same year, which has been regarded as a highly sensitive measure of population health.4 Preterm birth is the delivery of a baby before 37 weeks of gestation has been completed and has various sub categorizations, such as very preterm (28–32 weeks) and extremely preterm (<28 weeks).5 Due to uncertainty in precisely estimating gestation time, some countries categorize a preterm infant by birth weight of less than 2500g.5 One of the leading causes of infant mortality is birth defects. It is a term used for conditions of malformations, disruptions, or deformations that may be due to physical or biochemical abnormalities.6
The seven domains of health are all interconnected with infant mortality rates, but environmental, intellectual, and financial health are of particular relevance when analyzing the causes and stressors of infant mortality. Factors related to environmental health, such as the mother’s working environment and the presence of industrial pollution, can have a direct negative effect on the health of a fetus that can contribute to infant mortality.7 While intellectual health includes more than formal education, studies have found an association between low maternal education levels and an increased risk of infant mortality.8 Socio-economic status, or financial health, can have a significant effect on the overall health and well-being of the parent and infant. A study conducted in Nepal found that regions mainly composed of poor and middle-class individuals experienced higher infant mortality rates than the wealthier areas of the country.9 These three domains of health can all contribute to a lack of access to resources and support that may impact the likelihood of infant mortality.
Infant mortality rate can be an important indicator of population health when comparing the health status of countries or regions with the passage of time or at a single point in time. This information can also assist in guiding the allocation of health services and resources. For instance, Utah Pregnancy Risk Assessment Monitoring System (PRAMS) data indicate that parity, age, and education have notable effects on rates of infant mortality.2 Analyzing this information will allow for reflection on the current systems that are in place that may put certain populations at a disadvantage and make adjustments to better support them. While old and young age and lower education are well known risk factors for infant mortality,8 whether parity directly contributes to increased risk of infant mortality in Utah or is simply confounded by older age has yet to be explored. The main objectives of this data snapshot are to analyze the recent infant mortality trends in Utah and how they compare to national data. Additionally, we set out to evaluate the independent relationship between maternal parity and infant mortality in Utah, taking into account maternal age.
Methods
The data utilized for this analysis of infant mortality in Utah was collected from the years 2009 to 2019 for infants who died before their first birthday from Utah PRAMS via the Indicator-Based Information System for Public Health (IBIS-PH). PRAMS collects data directly from birth parents of live infants to provide estimates of various maternal and infant health indicators.10 Forty-six states, including additional US territories and local municipalities, participate in the surveys through funding and collaboration between the Centers for Disease Control and Prevention (CDC) and local health departments.11 The Utah Department of Health (UDOH) Reproductive Health Program manages the Utah division of PRAMS. Utah PRAMS conducts an annual survey to gain insights into maternal experiences before, during, and after pregnancy. The survey is administered based on a sampling system that randomly selects approximately 200 new mothers from Utah birth certificates two to four months after delivery.12 The data is stratified by birth weight and maternal education to highlight underrepresented groups.13
The outcome of interest was infants who died before their first birthday (under 365 days).
Data collected by Utah PRAMS was a pooled analysis spanning 10 years and included surveying maternal parity, age, and education levels. Response options to education level question included 8th grade or less; 9th–12th grade no diploma; high school graduate or GED completed; some college credit, but no degree; associate degree (e.g. AA, AS); bachelor’s degree (e.g. BA, AB, BS); master’s degree (MA, MS, MEng, Med, MSW, MBA); doctorate (e.g. PhD, EdD) or professional degree (e.g. MD, DDS, DVM, LLB, JD); none; or unknown. Deaths per 1,000 live births and 95% confidence intervals (CI) were reported for each education level. In our analyses assessing the relationship between parity and infant mortality, we accounted for confounding by maternal age via stratification.
Data and Results
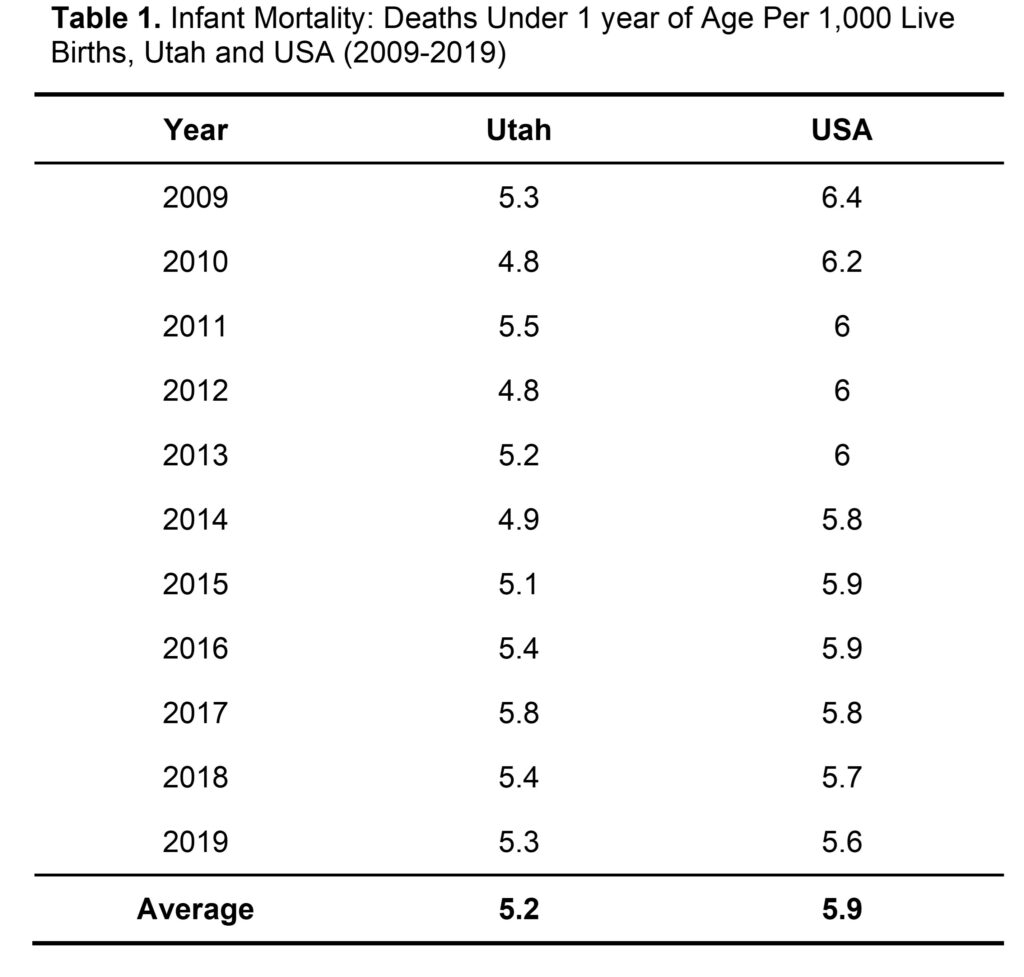
Between 2009 to 2019, Utah PRAMS collected information on 554,557 live births to Utah resident mothers regardless of where they occurred within Utah.14 Since the information related to live births in the Utah PRAMS database is collected from the birth and death certificates of the infants, it is difficult to gauge the number of women represented by the number of live births. Therefore, one woman might account for more than one live birth from 2009 to 2019. Of those live births, 2,834 resulted in infant deaths at 364 days or less.14 The study consisted of approximately 31.9% of women between the ages of 35 to 44, 33.4% of women between the ages of 20–34, and 34.8% of women between the ages of 15–19.14 The overall infant mortality rate in Utah from 2009 to 2019 was 5.2 infant deaths per 1,000 live births which was 0.66 fewer infant deaths per 1,000 live births than the US average (Table 1).
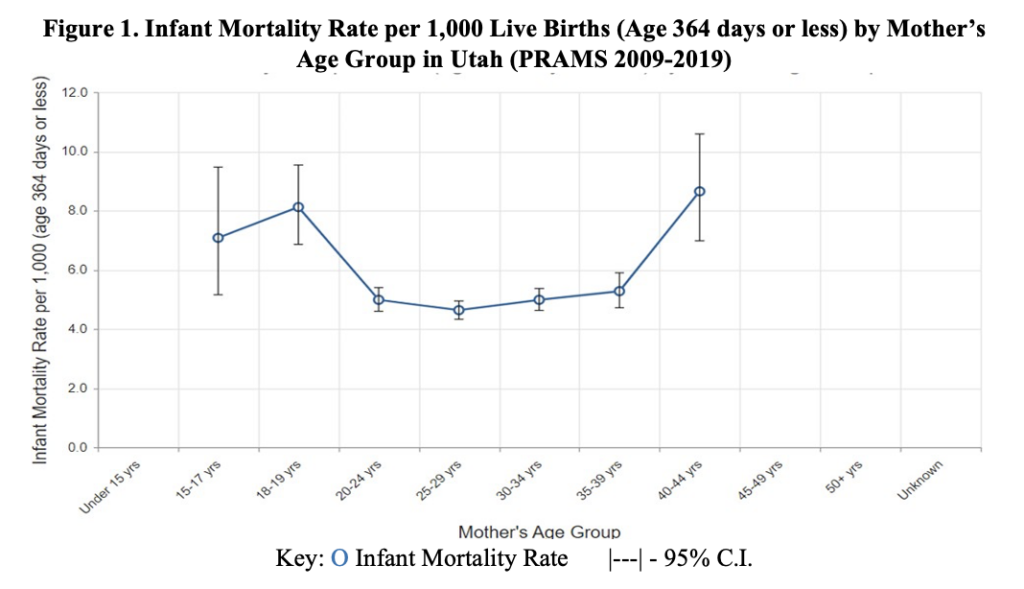
Despite a lower average infant mortality rate in Utah compared to the USA, higher infant mortality rates were prevalent among women aged 15–17, 18–19, and 40–44 years old in Utah (Figure 1). Mothers between the ages of 20–39 years old had an infant mortality rate of around 5 deaths per 1,000 live births. The infant mortality rate tends to be higher around critical moments of reproductive development in a woman’s life, such as puberty around the ages of 15–19 and the beginning stages of menopause which is around 40–44 years of age.15 These two phases demarcate the beginning and the end of the female reproductive life cycle.15
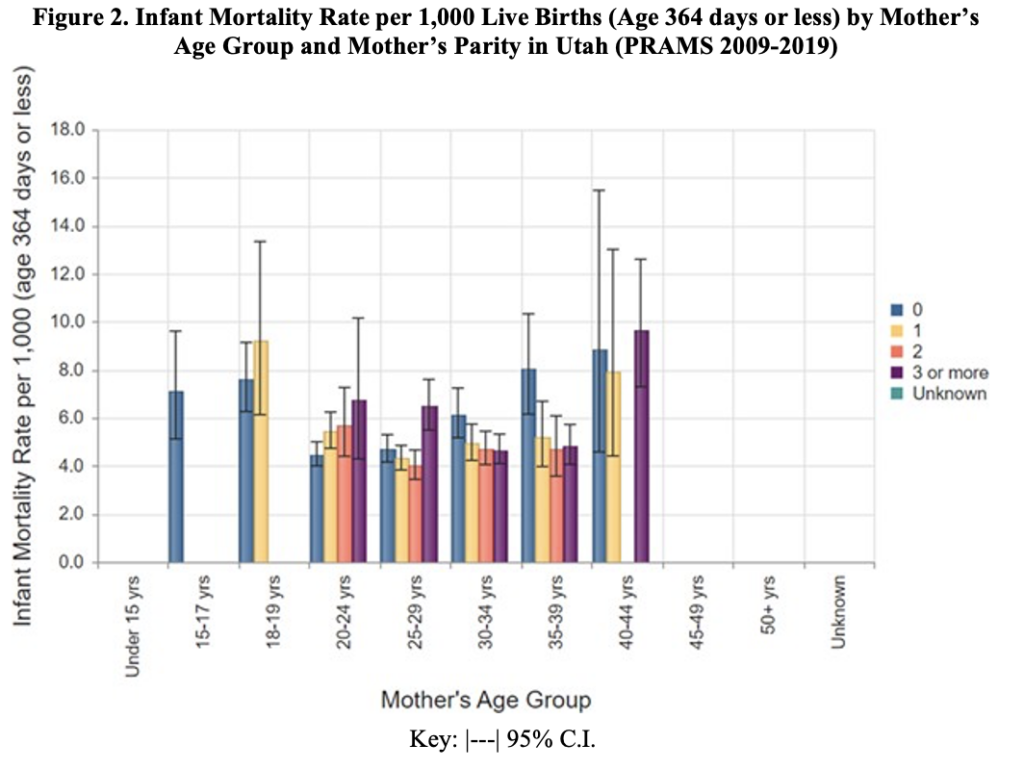
In the maternal age stratified analyses assessing relationship between parity and infant mortality (Figure 2), maternal age appears to be driving the relationship with a similar U-shaped relationship as seen in Figure 1. While 3+ parity showed the highest probability for infant mortality among women ages 25–29 and 40–44 years, nulliparous women had the highest probability of infant mortality among women ages 30–34 and 35–39 years. However, overlapping 95% CIs throughout the many comparisons indicate any direct association between parity and infant mortality is null.
In addition to age, there appeared to be a correlation between maternal education level and infant mortality rate. Women who reported only completing the 8th grade were twice as likely to experience an infant loss compared to those who held doctorates or professional degrees (Table 2). However, there was a steady decline in the probability of experiencing infant loss as each degree level increased. Mothers in the unknown category were the most susceptible group to experience infant loss, surpassing those who reported an education of 8th grade or less by an additional 4 deaths per 1,000 children (Table 2).

Discussion
The data analyzed in this snapshot of infant mortality between the years 2009–2019 in Utah has illustrated that women in the age groups 15–17, 18–19, and 40–44 years old experienced 3 more infant deaths per 1000 live births than 20–24, 25–19, 30–34, and 35–39-year-olds, on average. It should be noted that parity and infant mortality are confounded by age. Women aged 40–44 were identified as the most at-risk group for infant mortality. It is also essential to identify other high-risk groups, such as women who did not receive an education past the 8th grade and those in the 17–19 age group. Since Utah IBIS and PRAMS collected data on all live births in the state, the data analyzed gives the most accurate rates for Utah at the time.
Extreme maternal ages were notably associated with an increased risk of infant mortality. Biological maturation, sociodemographic factors like education, and economic factors play a role in adverse outcomes of adolescent and advanced maternal age pregnancies.16-18 These effects include an increased likelihood of infant mortality and adverse pregnancy and infant health outcomes.16-18 The negative impacts of advanced maternal age are also partly due to the link between increasing maternal age and a higher prevalence of pre-existing health conditions that may cause pregnancy complications, such as hypertension, obesity, placenta previa, gestational diabetes, etc.19 When considering interventions for these age groups, various biological and societal factors of each patient must be addressed to meet their needs.
As mentioned previously, a strength of PRAMS is its capacity to collect data that allows for a population-based analysis of all live births in Utah. However, the limitations of this analysis of infant mortality in Utah are linked to the limitations of the PRAMS database. Data from individuals who did not experience a live birth are not included in the PRAMS database. While infant mortality does not include stillbirths, comparing data on stillbirths and their possible causes to causes of infant mortality could have the potential to reduce the risk of both outcomes. Parity measures birth after at least 20 weeks of gestation in the US.20 If spontaneous or elective abortions occurred, data on that information was not collected by PRAMS to be factored into data on parity. The data regarding education was self-reported, so there could have been misreporting or a lack of reporting (Table 2).
Since there is a range of causes for infant mortality, a variety of prevention efforts would be necessary to decrease infant mortality rates. There is a strong association between infant mortality and maternal education.21 Therefore, education would be a powerful tool for both patients and healthcare providers to improve maternal and neonatal outcomes. The Utah Women and Newborn Quality Collaborative (UWNQC) aims to meet that goal by using “evidence-based practice guidelines and quality improvement processes.”22 The target populations for decreasing infant mortality based on the data analyzed from Utah PRAMS would be at the two ends of the U-shaped relationship between maternal age and infant mortality. This includes women between the ages of 15–17, 18–19, and 40–44. Utah offers a federally funded Personal Responsibility Education Program (PREP) that provides adolescents information on various pregnancy prevention interventions. Older women can seek advice at family planning clinics and programs to prevent pregnancies. The UDOH Maternal and Infant Health Program (UDOH-MIHP) also provides family planning services through the Mother to Baby Utah program. Prenatal counseling can be a useful tool to reduce infant mortality among pregnancies that are at risk for adverse health effects due to advanced maternal age. Genetic counseling could be further recommended to identify biomarkers that may increase the risk of infant mortality. The UDOH-MIHP is reviewing data compiled from public health programs to identify risks throughout the stages of pregnancy and develop corresponding programs to address those issues.2 Continued efforts on all fronts are crucial to reducing infant mortality in Utah as well as other populations.
References
- MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Semin Perinatol. 2011;35(4):200-208. doi:10.1053/j.semperi.2011.02.017
- Utah Department of Health, Center for Health Data and Informatics, Indicator-Based Information System for Public Health. Health Indicator Report of Infant Mortality. ibis.health.utah.gov. Published January 14, 2022. Accessed March 15, 2022. https://ibis.health.utah.gov/ibisph-view/indicator/view/InfMort.Ut_USYear.html
- Ely DM, Driscoll AK. Infant Mortality in the United States, 2018: Data From the Period Linked Birth/Infant Death File. Natl Vital Stat Rep. 2020;69(7):1-18. https://www.cdc.gov/nchs/data/nvsr/nvsr69/NVSR-69-7-508.pdf
- Reidpath DD, Allotey P. Infant mortality rate as an indicator of population health. J Epidemiol Community Health. 2003;57(5):344-346. doi:10.1136/jech.57.5.344
- Tucker J, McGuire W. Epidemiology of preterm birth. BMJ. 2004;329(7467):675-678. doi:10.1136/bmj.329.7467.675
- Kirby RS. The prevalence of selected major birth defects in the United States. Semin Perinatol. 2017;41(6):338-344. doi:10.1053/j.semperi.2017.07.004
- Genowska A, Jamiołkowski J, Szafraniec K, Stepaniak U, Szpak A, Pająk A. Environmental and socio-economic determinants of infant mortality in Poland: an ecological study. Environ Health. 2015;14:61. Published 2015 Jul 21. doi:10.1186/s12940-015-0048-1
- Anele CR, Hirakata VN, Goldani MZ, da Silva CH. The influence of the municipal human development index and maternal education on infant mortality: an investigation in a retrospective cohort study in the extreme south of Brazil. BMC Public Health. 2021;21(1):194. Published 2021 Jan 22. doi:10.1186/s12889-021-10226-9
- Khadka KB, Lieberman LS, Giedraitis V, Bhatta L, Pandey G. The socio-economic determinants of infant mortality in Nepal: analysis of Nepal Demographic Health Survey, 2011. BMC Pediatr. 2015;15:152. Published 2015 Oct 12. doi:10.1186/s12887-015-0468-7
- Shulman HB, D’Angelo DV, Harrison L, Smith RA, Warner L. The Pregnancy Risk Assessment Monitoring System (PRAMS): Overview of Design and Methodology. Am J Public Health. 2018;108(10):1305-1313. doi:10.2105/AJPH.2018.304563
- Centers for Disease Control and Prevention. (2022, January 21). Participating PRAMS Sites. Centers for Disease Control and Prevention. https://www.cdc.gov/prams/states.htm
- Utah Department of Health Maternal & Infant Health Program. Utah PRAMS. mihp.utah.gov. Published date unknown. Accessed March 14, 2022. https://mihp.utah.gov/pregnancy-and-risk-assessment
- Schliep KC, Denhalter D, Gren LH, Panushka KA, Singh TP, Varner MW. Factors in the Hospital Experience Associated with Postpartum Breastfeeding Success. Breastfeed Med. 2019;14(5):334-341. doi:10.1089/bfm.2018.0039
- Utah Department of Health, Center for Health Data and Informatics, Indicator-Based Information System for Public Health. Utah Death Certificate and Birth Certificate Databases. ibis.health.utah.gov. Updated December 10, 2021. Accessed March 15, 2022. https://ibis.health.utah.gov/ibisph-view/query/result/infmort/InfMortDeathLinkCnty/InfMortRate.html
- Hoyt LT, Falconi AM. Puberty and perimenopause: reproductive transitions and their implications for women’s health. Soc Sci Med. 2015;132:103-112. doi:10.1016/j.socscimed.2015.03.031
- Londero AP, Rossetti E, Pittini C, Cagnacci A, Driul L. Maternal age and the risk of adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):261. Published 2019 Jul 23. doi:10.1186/s12884-019-2400-x
- Driscoll AK, Ely DM. Effects of changes in maternal age distribution and maternal age-specific infant mortality rates on infant mortality trends : United States, 2000–2017. Centers for Disease Control and Prevention. https://stacks.cdc.gov/view/cdc/89876. Published June 25, 2020. Accessed July 18, 2022.
- Ratnasiri AWG, Lakshminrusimha S, Dieckmann RA, et al. Maternal and infant predictors of infant mortality in California, 2007-2015. PLoS One. 2020;15(8):e0236877. Published 2020 Aug 6. doi:10.1371/journal.pone.0236877
- Laopaiboon M, Lumbiganon P, Intarut N, et al. Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG. 2014;121 Suppl 1:49-56. doi:10.1111/1471-0528.12659
- Opara EI, Zaidi J. The interpretation and clinical application of the word ‘parity’: a survey. BJOG. 2007;114(10):1295-1297. doi:10.1111/j.1471-0528.2007.01435.x
- Cramer JC. Social factors and infant mortality: identifying high-risk groups and proximate causes. Demography. 1987;24(3):299-322. doi:10.2307/2061300
- Utah Department of Health Maternal & Infant Health Program. UWNQC Utah Women and Newborns Quality Collaborative. mihp.utah.gov. Published date unknown. Accessed March 14, 2022. https://mihp.utah.gov/uwnqc
Citation
Alsafi Z, Bartley S, & Kim S. (2022). An Overview Analysis of Infant Mortality in Utah: A Comprehensive Analysis of 2009–2019 Utah Pregnancy Risk Assessment Monitoring System (PRAMS) Data. Utah Women’s Health Review. doi: 10.26054/0d-2ya2-cnvg

