With the overturning of Roe v Wade by the Supreme Court on June 24, 2022, patients, advocates, clinicians, and researchers have braced themselves for the long-term negative impact on women’s health. The public and political discussion typically turns to abortion access and reproductive rights, with seldom consideration and conversation regarding how this decision may negatively impact the incidence of gynecological cancers, including ovarian cancer (OC). OC is defined as cancer of the ovaries and/or fallopian tubes and is the most lethal gynecological malignancy with a low five-year survival rate of ~29%-50% depending on the stage of diagnosis and subtype.1 Unlike cervical and breast cancers, OC currently lacks screening tools for early detection, contributing to late-stage diagnosis.2 Once diagnosed with OC, patients face substantial hurdles, including a lack of available treatment options and subjection to unnecessary side effects, due to a fundamental lack of understanding of this disease, resulting in ~70% of patients relapsing within three years.3 In general, cancer deaths in the US have slowly declined over the past few decades due to advances in research, medicine, and technology.4 However, it is feasible to presume that OC (and other gynecological cancers) mortality rates will increase due to the overturning of Roe v Wade, which will likely lead to decreased access to women’s health and reproductive health centers, a reduction in reproductive health education, fewer quality OBGYN’s and gynecological oncologists, and costly healthcare.
Access to women’s health and reproductive health centers will become severely limited, particularly in abortion restrictive states.5, 6 States that limit abortion access are apt to limit funding and/or shut down key organizations, such as Planned Parenthood, that provide affordable women’s healthcare.6 Beyond abortion access, Planned Parenthood offers annual checkups and screenings, immunizations, STI testing, birth control, education, primary care, cancer screenings, and more. Eliminating and/or limiting access to these healthcare centers will make it more challenging for women to seek fundamental healthcare and turning to general primary care doctors who may not be as well versed in women’s health and associated diseases. These organizations play a key role in prevention and initial access to OC diagnosis and treatment, which will suffer due to limited funding and resources, resulting in a higher OC mortality rate. Importantly, women’s health centers provide access to affordable oral contraceptive methods, which have a protective effect against OC.7 With decreased access to oral contraceptive methods, women will be at a higher risk for developing OC. Additionally, these centers provide access to genetic testing for patients with a family history of cancer, such as the BRCA mutation, which is associated with OC and breast cancer.8 Detection of a germline BRCA mutation at early ages can inform women, allowing them to take preventative measures, such as lifestyles changes, bilateral salpingo-oophorectomy (surgical removal of the fallopian tubes and ovaries), and double mastectomy (surgical removal of the breasts). These preventative measures can aid in decreasing the incidence and mortality rate of OC and breast cancer.9, 10 With limited access to women’s health and reproductive health centers, women will be less likely to receive genetic screening for the BRCA mutation, which will negate their ability to make informed preventative choices about their body, and ultimately result in a higher OC mortality rate. Additionally, women will likely be less educated about available genetic cancer testing and oral contraceptive methods in a post Roe v Wade world.5
Access to reproductive health education for patients, nurses, and clinicians will also likely decrease. Abortion restrictive states are censoring early education on reproductive biology due to political and religious agendas, creating challenges for women to make informed decisions about their bodies and to know when to seek care. Prior to the reversal of Roe v Wade, there was already an alarming lack of knowledge of the female anatomical system, with many Americans being unable to identify the number and location of the ovaries and/or fallopian tubes in women.11 Without having a basic understanding of the female anatomy, women face difficulties knowing when to seek help if they start displaying OC symptoms, especially not knowing what or where an ovary is! This is particularly problematic for vulnerable communities of women who already have limited opportunities and access to education.6 In Utah, high religious practice and cautious sexual attitudes have been associated with a negative intent to vaccinate children for HPV, which will likely increase cervical cancer incidence in the future.12 This same ideology may be translational to OC as parents may presumably impede on their children’s reproductive education and autonomy over their own bodies. The reversal of Roe v Wade will likely push female anatomy and reproductive health out of the health conversation for young children in abortion restrictive states and communities, negatively affecting their ability to make informed decisions for seeking care for OC diagnosis and treatment at later ages. This is further compounded by the increasing stigma surrounding women’s health in a post Roe v Wade landscape that may impede women speaking up and advocating for their health.
Access will be further thwarted by quality OBGYN’s and gynecological oncologists leaving or avoiding abortion restrictive states and moving to abortion protective states.13 In addition, it is predicted that medical and nursing staff will receive less formal training and education on women’s health in abortion restrictive states, which may negatively impact OC.6 This will increase the cost and distance that women have to travel to receive quality care as well as limited access to clinicians. Due to the complexities of OC, patients’ outcomes can be highly correlated to the expertise of their gynecological oncology specialist. Late-stage diagnosis of OC is attributed to asymptomatic or vague symptoms, such as abdominal fullness, bloating, abdominal pain, and GI symptoms, which can be commonly misdiagnosed by healthcare providers with proper identification of symptoms occurring in ~59%-93% of OC cases.2, 14 With fewer available women’s health clinics and specialists in rural abortion restrictive states, it is reasonable to believe that women will be misdiagnosed and less likely to receive initial OC diagnosis, delaying treatment and ultimately increase the mortality rate of OC.
The economic cost and burden on patients to access OC diagnosis and treatment in abortion restrictive states will increase following the overturn of Roe v Wade. OC treatment costs ~$100,000 in the first year following surgery and predominately serves Non-Hispanic White (NHW) women who on average have the highest socioeconomic status, which is attributed to racial disparities in the US.15, 16 The overturning of Roe v Wade will increase the associated costs of OC treatment and widen the inequities for accessing OC diagnosis and care, increasing the OC mortality gap across groups of women. This will particularly negatively affect marginalized communities of women, such as Black women, who already have a ~18-29% higher OC mortality rate compared to NHW women.5, 15 Prior to the overturning of Roe v Wade, women were already traveling hundreds of miles from around the mountain west states to see specialists at the Huntsman Cancer Institute at the University of Utah for OC diagnosis and treatment. Women will now have to travel greater distances for access to quality OBGYN’s and OC specialists, and many of whom do not have the means to.17 This will place more of a financial burden on abortion protective states and create long wait times to see specialists, delaying subsequent OC diagnosis and treatment.17 Furthermore, the emotional and time consuming demands of the influx of patients on quality OC healthcare providers in these areas may negatively affect their ability to diagnose and treat patients.17 Finally, advancements in OC research will decrease due to a lack of funding opportunities in abortion restrictive states. OC is a disease with a tremendous unmet need for new treatments and a further lack of funding as an outcome of Roe v Wade will severely affect future OC developments.
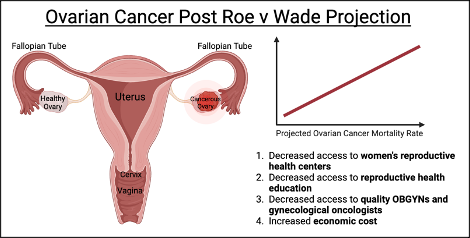
Reversing Roe v Wade has negative implications on abortion access for women across the country making every aspect of women’s health less accessible and more vulnerable, including OC. OC mortality rates will likely increase, especially in abortion restrictive states, due to decreased access to women’s health and reproductive health centers, a reduction in reproductive health education, fewer quality OBGYN’s and gynecological oncologists, and costly healthcare. These negative outcomes will have a stronger effect on vulnerable communities of women who already have a higher risk of OC mortality.15 To overcome these challenges, it is paramount that researchers and clinicians work tirelessly to raise funding, increase education, and awareness of this disease as well as work with policy makers to protect women’s reproductive health, especially in vulnerable communities of women and in abortion restrictive states such as Utah.
Table of Contents
References
- Torre LA, Trabert B, Desantis CE, Miller KD, Samimi G, Runowicz CD, Gaudet MM, Jemal A, Siegel RL. Ovarian cancer statistics, 2018. CA: A Cancer Journal for Clinicians. 2018;68(4):284-96. doi: 10.3322/caac.21456.
2. Wallis B, Bowman KR, Lu P, Lim CS. The Challenges and Prospects of p53-Based Therapies in Ovarian Cancer. Biomolecules. 2023;13(1):159. PubMed PMID: doi:10.3390/biom13010159.
3. Ramraj SK, Elayapillai SP, Pelikan RC, Zhao YD, Isingizwe ZR, Kennedy AL, Lightfoot SA, Benbrook DM. Novel ovarian cancer maintenance therapy targeted at mortalin and mutant p53. International Journal of Cancer. 2020;147(4):1086-97. doi: 10.1002/ijc.32830.
4. Hulvat MC. Cancer Incidence and Trends. Surg Clin North Am. 2020;100(3):469-81. Epub 20200327. doi: 10.1016/j.suc.2020.01.002. PubMed PMID: 32402294.
5. Coen-Sanchez K, Ebenso B, El-Mowafi IM, Berghs M, Idriss-Wheeler D, Yaya S. Repercussions of overturning Roe v. Wade for women across systems and beyond borders. Reproductive Health. 2022;19(1):184. doi: 10.1186/s12978-022-01490-y.
6. Berg JA, Woods NF. Overturning Roe v. Wade: consequences for midlife women’s health and well-being. Womens Midlife Health. 2023;9(1):2. Epub 20230106. doi: 10.1186/s40695-022-00085-8. PubMed PMID: 36609311; PMCID: PMC9824972.
7. Bosetti C, Negri E, Trichopoulos D, Franceschi S, Beral V, Tzonou A, Parazzini F, Greggi S, La Vecchia C. Long-term effects of oral contraceptives on ovarian cancer risk. International Journal of Cancer. 2002;102(3):262-5. doi: https://doi.org/10.1002/ijc.10696.
8. Elezaby M, Lees B, Maturen KE, Barroilhet L, Wisinski KB, Schrager S, Wilke LG, Sadowski E. BRCA Mutation Carriers: Breast and Ovarian Cancer Screening Guidelines and Imaging Considerations. Radiology. 2019;291(3):554-69. doi: 10.1148/radiol.2019181814. PubMed PMID: 31038410.
9. Hanley GE, Pearce CL, Talhouk A, Kwon JS, Finlayson SJ, McAlpine JN, Huntsman DG, Miller D. Outcomes From Opportunistic Salpingectomy for Ovarian Cancer Prevention. JAMA Network Open. 2022;5(2):e2147343-e. doi: 10.1001/jamanetworkopen.2021.47343.
10. Mau C, Untch M. Prophylactic Surgery: For Whom, When and How? Breast Care (Basel). 2017;12(6):379-84. Epub 20171213. doi: 10.1159/000485830. PubMed PMID: 29456469; PMCID: PMC5803721.
11. Reid J, Brueggmann D, Templeman C, Jaque J. AWARENESS AND UNDERSTANDING OF FEMALE PELVIC ANATOMY AND CLINICAL APPLICATIONS AMONG OBSTETRIC AND GYNECOLOGY PATIENTS AT LAC+USC. Contraception. 2014;90(2):198. doi: 10.1016/j.contraception.2014.06.013.
12. Redd DS, Jensen JL, Bodily RJ, Lee AA, Skyles TJ, Poole BD. Cautious Sexual Attitudes Diminish Intent to Vaccinate Children against HPV in Utah. Vaccines. 2022;10(9):1382. PubMed PMID: doi:10.3390/vaccines10091382.
13. Woodcock AL, Carter G, Baayd J, Turok DK, Turk J, Sanders JN, Pangasa M, Gawron LM, Kaiser JE. Effects of the Dobbs v Jackson Women’s Health Organization Decision on Obstetrics and Gynecology Graduating Residents’ Practice Plans. Obstetrics & Gynecology. 2023;142(5).
14. Goldstein CL, Susman E, Lockwood S, Medlin EE, Behbakht K. Awareness of symptoms and risk factors of ovarian cancer in a population of women and healthcare providers. Clin J Oncol Nurs. 2015;19(2):206-12. doi: 10.1188/15.Cjon.206-212. PubMed PMID: 25840386.
15. Gomez SL, Chirikova E, McGuire V, Collin LJ, Dempsey L, Inamdar PP, Lawson-Michod K, Peters ES, Kushi LH, Kavecansky J, Shariff-Marco S, Peres LC, Terry P, Bandera EV, Schildkraut JM, Doherty JA, Lawson A. Role of neighborhood context in ovarian cancer survival disparities: current research and future directions. American Journal of Obstetrics and Gynecology. 2023;229(4):366-76.e8. doi: https://doi.org/10.1016/j.ajog.2023.04.026.
16. Bercow AS, Chen L, Chatterjee S, Tergas AI, Hou JY, Burke WM, Ananth CV, Neugut AI, Hershman DL, Wright JD. Cost of Care for the Initial Management of Ovarian Cancer. Obstet Gynecol. 2017;130(6):1269-75. doi: 10.1097/aog.0000000000002317. PubMed PMID: 29112648; PMCID: PMC5709160.
17. Rubin R, Abbasi J, Suran M. How Caring for Patients Could Change in a Post Roe v Wade US. JAMA. 2022;327(21):2060. doi: 10.1001/jama.2022.8526.
Citation
Wallis, B. (2024). 7 Domains of Women’s Health: Ovarian Cancer Landscape Post Roe v Wade. Utah Women’s Health Review.

