Background
A recent study by the Utah Commission on Criminal and Juvenile Justice [1] indicated that 12-13% of Utah women reported being raped at some point in their lives. Nationally, CDC estimates suggest that 1 in 6 women (16.6%) report experiencing an attempted or completed rape at some point in their lives.2 In 2003, 793 rapes were reported in Utah. Since it is estimated that only 20% of victims report the crime to law enforcement in the state [1], the actual number may approach 4,000 rapes each year. The consequences of rape include unwanted pregnancy and sexually transmitted disease, including HIV. An estimated 5% of sexual assaults result in pregnancy, and 33% may results in sexually transmitted disease [2]. Public health and other expert recommendations include counseling all sexual assault patients at risk of pregnancy about emergency contraception and providing it as an option on-site. Treatment for sexually transmitted diseases should also be discussed and offered [3].
Methods
In order to determine if Utah hospitals are meeting these standards, a coalition of health care and advocacy groups (the Utah Sexual Assault Safety Project) contacted all 42 Utah hospitals with emergency departments. Surveys were completed with 41 of those hospitals. Telephone interviews were conducted with emergency room personnel most familiar with the protocols for sexual assault patients. Most often this was a sexual assault nurse-examiner (SANE nurse) or the nurse manager. The survey consisted of 10 open- and close-ended questions designed to determine the services that are provided routinely to victims of sexual assault [3].
Results
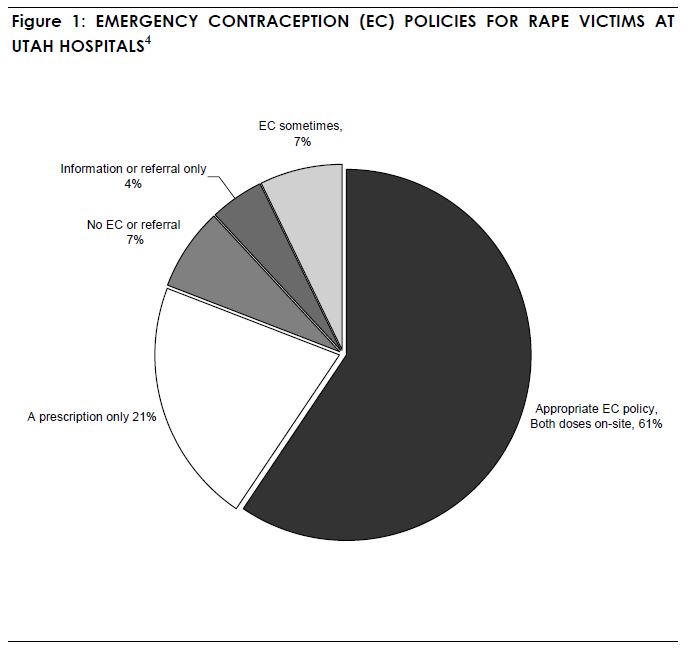
Only 60% of sexual assault victims receive consistent and appropriate services on-site. (See Figure 1). Most Utah hospitals are providing treatment for sexually transmitted diseases (STD) to sexual assault victims. (See Figure 2).
Summary and Needs
Hospital emergency departments are often the first contact victims have when seeking help, and it is therefore critical that emergency room personnel provide rape victims with comprehensive services that include emergency contraception as well as the diagnosis and treatment for sexually transmitted diseases. This survey indicates that there is room for improvement: 40% of the emergency departments in Utah do not consistently meet the standard for treating rape victims.
The Utah Sexual Assault Safety Project will provide information and training to hospitals that do not currently provide comprehensive services to victims. There should be additional funding and training to increase the number of SANE nurses where primary treatment occurs.
References
- Utah Commission on Criminal and Juvenile Justice Research and Data Unit. “Rape in Utah: A Survey of Utah Women’s Experience”. 2005. Available from http://www.justice.utah.gov/Research/SexOffender/RapeInUtah.pdf. Accessed 11/14/06
- National Center for Injury Prevention and Control, Centers for Disease control. “Sexual Violence” 2006. Available from www.cdc.gov/ncipc/factsheets/ svfacts.htm. Accessed 11/14/06
- 2002 national guidelines on the management of adult victims of sexual assault. National Guideline Clearinghouse. Available from: http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=3050&nbr=2276 Accessed 11/14/06.
- Survey and Data by the Utah Sexual Assault Safety Project, Fall 2005. Available from http://www.acluutah.org/ecreport.pdf. Accessed 11/14/06