Table of Contents
Abstract
Objectives: Perinatal depression is a serious condition that many women experience in Utah. Women with this challenge may not receive adequate treatment even when they are screened. This study evaluated the needs of Utah women who are perinatally depressed and identified recommendations for addressing this public health concern.
Methods: Data collected from the Utah PRAMS survey on 8,491 women were analyzed. Of these women, 307 had depressive symptoms and provided substantive comments to the open-ended question. Multivariate logistic regression analysis was performed. The results were expressed as adjusted odds ratios. A qualitative analysis of the open-ended responses was also executed to identify various thematic categories.
Results: Women from a non-white background, women who were not married, and women with lower socioeconomic status had higher odds of experiencing depressive symptoms. In the thematic analysis, most women wished they had received better medical care during pregnancy or at delivery and several described an unmet need related to their depressive symptoms. Many women experienced diseases during the perinatal period while others had a positive pregnancy experience or delivery.
Conclusion: Race, marital status, and socioeconomic status may increase the odds for women in Utah to have postpartum depression. In addition, Utah women with perinatal depression continue to have unmet needs for diagnosis and treatment.
Implications: Though screening services for postpartum depression have improved, Utah should increase the frequency and consistency of screening, provide more training about identifying perinatal depression to nurses and other healthcare professionals, and support integrated behavioral healthcare models to treat perinatally depressed mothers.
Introduction
Perinatal depression is a mood disorder experienced by many women during pregnancy and the postpartum period of 12 months after delivery.1,2,3,4,5,6,7 The American College of Obstetricians and Gynecologists (ACOG)1 indicates that one in seven women will be diagnosed with depression during the perinatal period. Women with perinatal depression may suffer symptoms such as loss of interest, suicidal thoughts, and feeling distant from the baby.3,5,8 The presence of any of these symptoms is associated with major depressive episodes. Diagnosis occurs through screening during regular pregnancy check-ups with a physician. Once diagnosed, women with perinatal depression need resources to receive optimal treatment.
Data collected from the Pregnancy Risk Assessment Monitoring System (PRAMS) survey in Utah show that depression and anxiety rates among pregnant women increased between 2016 and 2020.9 Furthermore, the 2020 Utah statewide needs assessment for maternal and child health indicated that perinatal depression is an issue and that the state needs to expand mental health services to address this disorder.10 The purpose of this study was to evaluate the current needs of women suffering with perinatal depression in Utah and identify approaches to provide them with better healthcare services.
Methods
This is a mixed methods study of data collected from the Utah PRAMS survey from 2016 to 2021. The CDC collects data on maternal attitudes and experiences before, during, and after pregnancy.11 States are permitted to add their own questions to the PRAMS survey with CDC approval. Utah has added questions related to anxiety and depression based on the needs of mothers in Utah. Women completing the survey have an opportunity to respond to an open-ended question as well. This study is a secondary analysis of Utah PRAMS data and a thematic analysis of qualitative data collected from the open-ended question. A total of 8,491 women completed the Utah PRAMS survey from 2016 to 2021. Of these women, 1,715 responded to the open-ended question at the end of the survey. The inclusion criterion for the thematic analysis was that the women had depressive symptoms based on their responses to two survey questions on the PRAMS survey. After removing comments that were unsubstantial, 307 respondents remained.
Dependent Variable
The dependent variable in this study was having depressive symptoms. A survey participant who had depressive symptoms was a variable generated in the PRAMS dataset based on the participants’ responses to the following questions:
- Since your new baby was born, how often have you felt down, depressed, or hopeless?
- Since your new baby was born, how often have you had little interest or little pleasure in doing things you usually enjoyed?
Responses to these questions were limited to “Never”, “Rarely”, “Sometimes”, “Often”, and “Always”. Women who indicated at least “Sometimes” for both or either of these questions were considered to have some level of depressive symptoms, though specific variation was not measured. Responses were combined into the variable “depressive symptoms”.
Independent Variables
The two questions directly contributing to the outcome variable were used in the analysis because one study described symptoms of PPD to include depressed mood and diminished interest or pleasure in activities.12 This study also found that PPD is likely underreported because of the stigma surrounding mental health and being perceived as a good mother.12 Other risk factors from the literature were considered in determining which independent variables to include in the analysis, such as social and cultural factors,12,13,14 including age, marital status, race, Hispanic background, and income percentage of the Federal poverty line. The latter of these variables was considered a proxy variable for income. Similarly, insurance status was included as a socioeconomic variable due to its relationship to income and education.
Much of the literature indicated that screening services need improvement and more consistency across clinics.12,15,16,17,18 Because untreated depression can lead to the mother taking her life or harming the child,12 and if a woman is not receiving adequate screening in the perinatal period, she may be more susceptible to escalating depressive symptoms. Thus, screening was a focal point of the analysis and was distinguished between screening during the prenatal visit and screening at the postpartum visit.
Quantitative and Qualitative Analyses
Logistic regression was used to analyze the categorical variables coded into ordinal data. Three models were built using different combinations of independent variables. While no models incorporated every response variable from the PRAMS Phase 8 survey, Model 1 utilized the most independent variables as listed in Table 2, excluding whether the patient sought help for their perinatal depression. Model 2 included the three options for the insurance status variable. The aim was to isolate the group of individuals who had private/group insurance versus Medicaid. In this same model, the patient’s response about asking the physician for help was incorporated as an essential component of mental health stigma. Model 3 removed the additional variables in Model 2, including the percentage of the federal poverty line and Hispanic background status. The intention of this model was to isolate the race variable to determine whether it was more related to the outcome while excluding ethnicity as a potential confounder. Stata version 15.1 was used to analyze the quantitative data.
For the qualitative data, each individual response was read and evaluated. Based on the general theme of the response, a code was assigned. Some of these codes were combined into larger thematic categories after the initial assignment. Other codes had many responses without recategorizing them into broader groups. Dedoose software was used to identify themes in the open-ended responses and summarize all the data.
Results
Quantitative
Table 1 shows all the characteristics of the survey participants for select categories from 2016-2021. Most women who completed the survey were white and of a non-Hispanic background (85.96% and 81.13% respectively). Many of them had at least a high school diploma (27.3%) and several had a college degree (42.9%). Likewise, the sample included more women with higher incomes, at least 185% of the Federal Poverty Line or higher (58.16%). A high number of women had private/group insurance (70.09%) compared to those who had Medicaid or no insurance (26.57%) and a lower percentage of women were eligible for WIC during their pregnancy (23.05%). These were characteristics considered as independent variables that could influence the outcome variable of PPD symptoms.
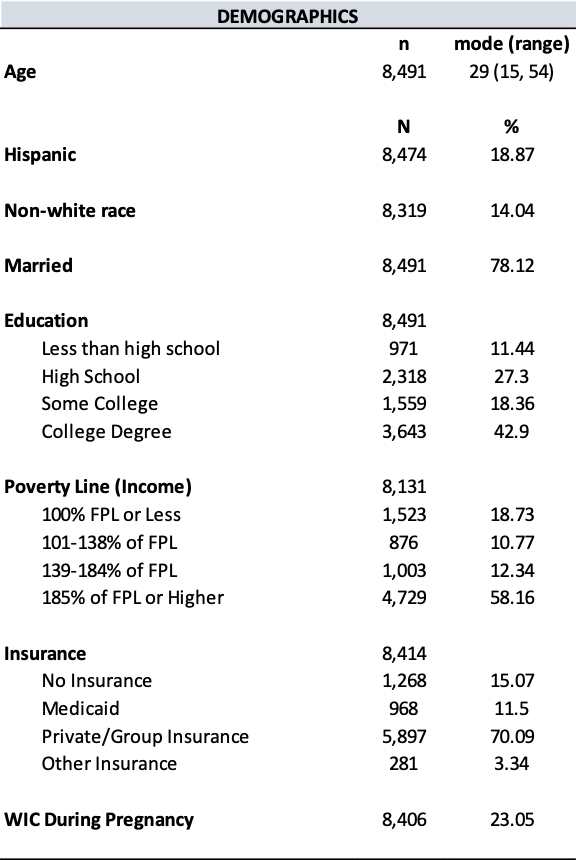
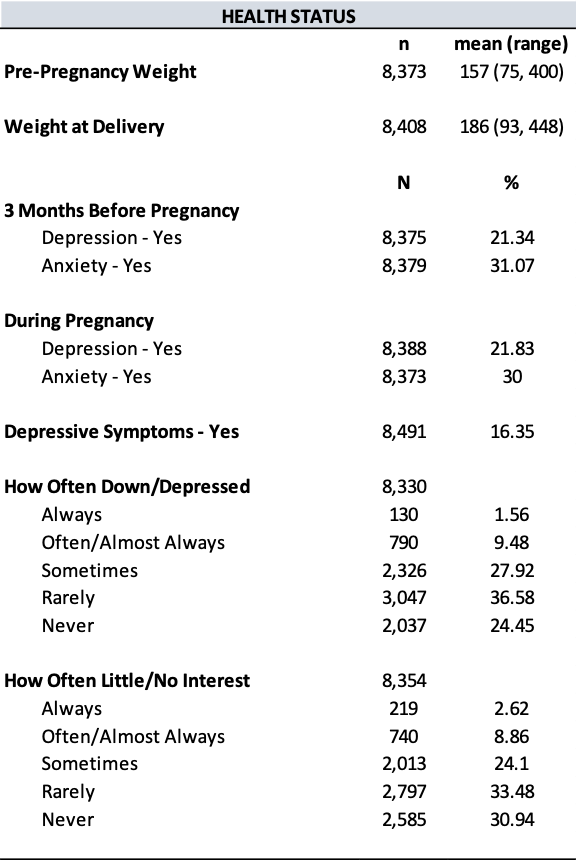
The most frequent age of survey participants was 29 years old, ranging from as low as 15 years and as high as 54 years. The average weight before pregnancy was 157 pounds and average weight at delivery was 186 pounds. A small proportion of women had depression three months before pregnancy (21.34%), while only 16.35% of women had depressive symptoms based on their responses to two dependent variable questions.
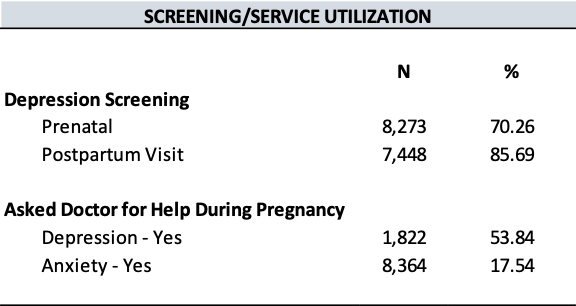
Other important characteristics to note are related to screening services. When it comes to depression screening, 70.26% of women received screening during their prenatal visit and 85.69% received screening at their postpartum visit. While many women responded to the question about whether they asked their doctor for help with anxiety at some point during their pregnancy, only 1,822 (21.46%) of participants answered the question about seeking help for depression during pregnancy, perhaps because of mental health stigma or the belief that doctors would not take them seriously.
Table 2 shows the results of the logistic regression. Both variables that directly determined the outcome variable were statistically significant in every model. Notably, women with a household income equivalent to a higher percentage of the Federal Poverty Line had a decreased odds of experiencing depressive symptoms since delivering their baby (OR = 0.8641, p = 0.06). In other words, women with a higher income were less likely to have depressive symptoms. This was statistically significant only in Model 1, which excluded whether the patient asked for help for their depression during pregnancy and the breakdown of insurance status categories. In contrast, Model 2 showed that women with a higher percentage of the Federal Poverty Line had an increased odds of PPD symptoms (OR = 1.1862) but was not statistically significant. Another variable statistically significant was women who had private or group insurance in Model 2. Women with this type of insurance had a decreased odds of having PPD symptoms after delivery (OR = 0.3651, p = 0.03) compared to women with other types of insurance (OR = 0.6259 for Medicaid and 0.3784 for other insurance).
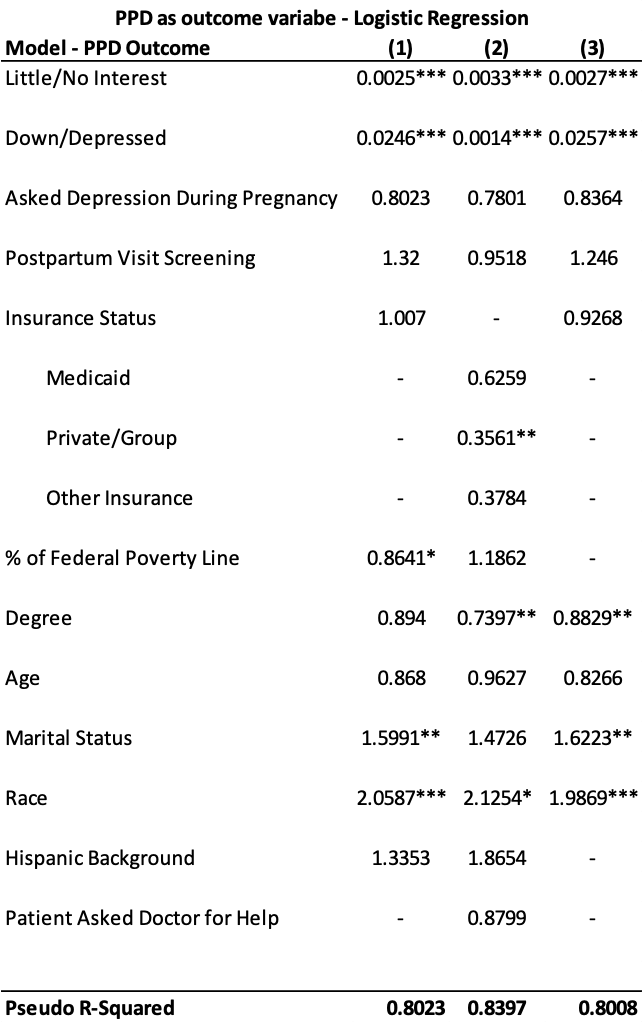
* p < 0.10
** p < 0.05
*** p < 0.002
Variables that were statistically significant for more than one model included degree level, marital status, and race. Women with a higher educational level had a decreased odds of experiencing depressive symptoms (OR = 0.7397 and OR = 0.8829, p = 0.03). In contrast, women who were not married had an increased odds of PPD symptoms (OR = 1.5991 and 1.6223, p = 0.02). Interestingly, race was the only variable statistically significant in every model, suggesting that race has a relationship with depressive symptoms. In all scenarios, being a non-white race resulted in an increased odds of experiencing depressive symptoms in the postpartum period (OR = 2.0587 and 1.9869, p = 0.002 and p = 0.001; OR = 2.1254, p = 0.09). This remained statistically significant even after removing Hispanic background status from the model.
Qualitative
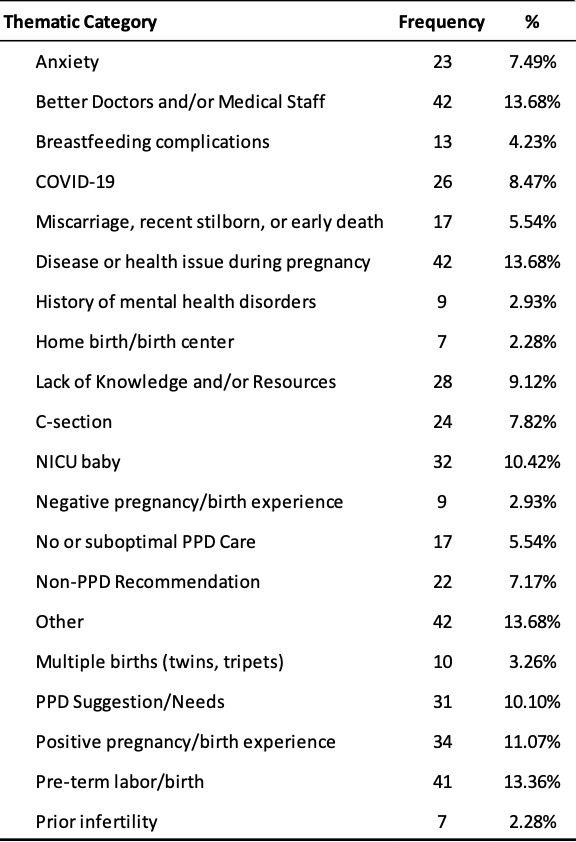
Based on the analysis of 307 open-ended responses from women who had depressive symptoms, 20 thematic categories were identified. Figure 1 shows the top five categories. The “Other” category was a broad theme that consisted of responses relating to the participant’s unique circumstances or general advice for other expecting mothers.
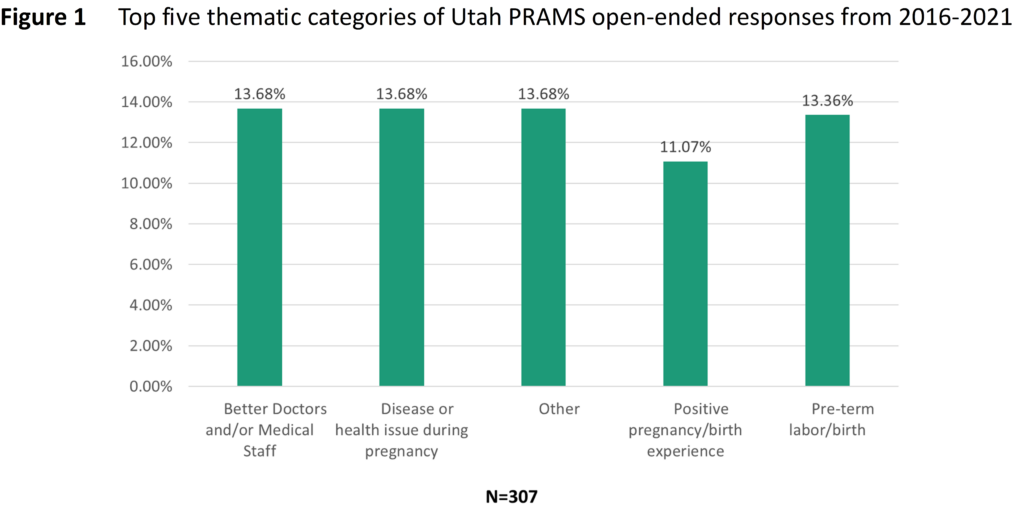
Table 3 summarizes the frequency of comments that fit into the 20 categories. Although there were 307 responses that met the criteria of this study, they could have fallen into more than one category, meaning each category totals a number greater than 307. In addition to the categories shown in Figure 1, other relevant categories worth noting include having a NICU baby (10.42%), unmet needs related to postpartum depression (10.10%), and lack of knowledge or resources (9.12%).
Better doctors or medical staff
Many women with depressive symptoms expressed that they were disappointed with the type of care they received from their doctor during pregnancy or at the hospital from nurses and other healthcare professionals. One woman explained that she felt pressured by her OB/GYN to deliver by cesarean. This made her feel uncomfortable and she ended up delivering vaginally with no complications. However, she was distressed that her physician was not sensitive or compassionate to her needs.
Other women described symptoms of depression and anxiety after delivery and not being prepared for that. There is insufficient follow-up and support during the perinatal period and women are left feeling alone and helpless after their baby arrives.
“It is a little upsetting to me that there isn’t enough follow-up care or discussion with the mother’s regarding PPD here in Utah. I have NEVER filled out a survey or been asked about my thoughts & well-being after having a baby…. Also, a little discussion and concern for the mother…. Moms are exhausted and doing so much for their babies and family. It would be nice if someone was concerned & looking out for mom every once in a while. A lot of women, like myself, don’t even know they have PPD. Please help us Moms!“
Having feelings of guilt and shame are likely enhanced by mental health stigma. Women may not feel like they are adequate mothers when they experience symptoms of depression or anxiety. Consequently, healthcare professionals should consider reassuring their patients that these feelings are normal, though difficult to cope with. These women can feel better with proper treatment and follow-up. Yet many women with depressive symptoms in this study did not experience follow-up and highlights a critical unmet need.
Disease or health issue during pregnancy
While not as prevalent as the need for better, compassionate healthcare professionals, many women mentioned how they suffered a disease or health condition during pregnancy, including hyperemesis gravidarum, preeclampsia, an incompetent cervix, or COVID-19. Hyperemesis gravidarum and preeclampsia were the most prevalent. Part of the problem with developing any disease during pregnancy is when women do not believe they receive sufficient resources. One participant suggested that Utah should have more resources specifically for expectant mothers with hyperemesis gravidarum.
Coping with the additional stress of these diseases could lead to other complications during pregnancy or birth. Increased stress could lead to pre-term labor or delivery, which also has an increased chance of having a baby with a medical issue that requires a stay in the NICU. Women with these diseases during pregnancy mentioned feelings of distress and worry. Thus, it is important for public health professionals in Utah to evaluate the need for developing more resources for diseases such as hyperemesis gravidarum or preeclampsia, especially if it can help women navigate their struggle with a trained physician who cares and understands.
Positive pregnancy or birth experience
Interestingly, many of the comments related to the survey respondents having a positive birth experience or pregnancy. This category also notably had more native Spanish-speaking women, so it would be interesting to see if women with a Hispanic background experience perinatal care or mental health struggles differently. In general, women with positive pregnancy or birth experiences may have chosen to not focus on underlying risk factors. It is also possible that they had a stronger support system.
“I have enjoyed it since labor and all is due to relax on my side of motherhood and not being stressed and having the support on both sides, partner and husband and family that is very important to me that keeps postpartum [depression] away for the mother.“
Conversely, the lack of a support system could be a contributor to depressive symptoms. The quantitative analysis of this study found that women who were married had a decreased odds of experiencing PPD. Although marital status is not the only indicator of a support system, having a partner, friends, or other family who can help take care of the new baby and ensure the mother receives time to relax is beneficial.
Unmet needs related to postpartum depression
Overall, women continue to have unmet needs when it comes to their perinatal care. Some women expressed that postpartum care and education is necessary and that more than one checkup after birth is essential. As one woman put it, “[O]ur mental health matters too.” Similarly, other women felt like doctors did not talk enough about PPD during their prenatal visits, and they did not know why. This could be because doctors have limited time with patients, so it may be worth providing additional training to nurses and other frontline staff who spend more time with patients. If they know what symptoms to look for, they may be able to identify them in the patient before a doctor does. They also tend to be the employees who administer the screening tool.
As it relates to screening, some women never received any and others felt that the survey process was insufficient. “[Postpartum depression screening] felt like a simple record keeping thing and not something they were willing to help with. I hope that PPD/A is taken more seriously in the future by all providers.” This comment suggests that even if screening increases, healthcare professionals need additional training to know what to do with the information and to also connect patients with the treatment they need.
Finally, women feel like their mental health challenges go unnoticed or are not taken seriously. One respondent explained, “I felt dumb and that my feelings and thoughts would get better by the way I was brushed off…I think more women suffer with this and are afraid to say something & when you build up the nerve to finally say something and not feel heard it was hard.” They likely deal with mental health stigma, which is unique to mothers who are held to traditional values and standards. Women who feel shame, guilt, or embarrassment about their feelings may not feel comfortable enough to share their feelings. As this respondent noted, when their voices are not heard, then they will not share them with healthcare professionals in the future, which can impact their depressive symptoms.
Discussion and Health Implications
This study supported the need for improved healthcare and resources for women in the perinatal period, which aligns with the findings of the Utah statewide maternal and child health needs assessment.10 Race, marital status, and socioeconomic status were found to increase the odds for postpartum depressive symptoms. While non-white women had an increased odds of having depressive symptoms in this study, Utah PRAMS data generally shows a gap in the prevalence of PPD between white and non-white populations, with white populations experiencing a higher prevalence.19
Moreover, studies have shown that marital satisfaction and peer and family support are risk factors for PPD.13,20 Other studies have found that socioeconomic status has a relationship with PPD.12,13,20 In these studies, lower socioeconomic status (lower income and lower education) was identified as a risk factor for PPD, which supports the findings of increased odds ratios in this study.
Stressful life events, limited resources, and deficient prenatal health knowledge may also be related to a woman developing PPD symptoms. Two studies have found that all these factors can have an increased risk for PPD.14,20 In this study, participants in the Utah PRAMS survey described difficult life experiences, including the presence of disease during pregnancy, and little knowledge of what to expect during the perinatal period.
While Utah currently has a Maternal Mental Health Toolkit and a website to help women find a mental healthcare professional, challenges continue to exist related to physician and nurse training, screening services, and connecting patients to healthcare professionals who can treat mental health struggles. Though not specific to Utah, some studies have shown that nurses feel underprepared to meet the needs of perinatally depressed patients.16,21 At least one study found that inadequate training can lead to poor screening practices.16 Thus, providing better education and training to nurses and other healthcare professionals could help improve PPD screening.
Although Utah’s screening rates at the postpartum visit have improved from 2016 to 2021,19 there remains inconsistency in screening practices. This may be related to the amount of screening tools available. Even though Utah has improved depression screening at the postpartum visit, screening needs to occur more frequently. UDHHS encourages expanding ACOG’s recommendation1 so that screening takes place at the first visit, each trimester, one to two days postpartum, two weeks postpartum, six weeks postpartum, and at each well-baby check for one year postpartum.22
Additionally, healthcare professionals should consider implementing integrated behavioral healthcare (IBH). IBH is a model used to create more collaborative efforts to address mental health issues when patients visit with their primary care provider. By bringing together professionals from various fields of expertise through an IBH manager, patients can receive more targeted approaches to their healthcare that yields more quality care. IBH programs are an efficacious means for bridging gaps between women in the perinatal period and their healthcare providers.23 IBH can also address fragmentation in perinatal mental health services.24
Strengths and Limitations
The strengths of this study included the high volume of responses included as well as the review of both quantitative and qualitative data that provided mutual support of the outcomes. Given the large sample of Hispanic and low SES survey participants in this study, results may be generalizable to these populations. However, this study was limited to Utah participants in the PRAMS survey, thus the findings may not be generalizable to all populations, including those in other states or countries. Another limitation to this study is the difficulty in measuring health equity. Most women who completed the survey had at least a college degree and identified as white. The PRAMS survey does not ask about sexual orientation, which would also be an important consideration for future phases of the PRAMS project.
While this study assessed the importance of screening, there were no questions on the PRAMS Phase 8 survey that looked at treatment of perinatal depression. Thus, the ability to assess discrepancies between women screened and treated versus women who were screened and not treated is limited. Since the Phase 9 survey began, a new question was added to solicit responses in this area now. Another confounder not considered in this study that should be evaluated in the future is the possibility of risk factors increasing the odds of screening taking place, such as low SES, disease during pregnancy, or depression prior to pregnancy. Other studies should also look at whether the failure to screen and treat women is a result of a poor screening process or the lack of available resources to effectively do so.
Conclusion
More information should be collected during the perinatal period to determine the severity of depression during pregnancy in addition to the postpartum period. Although screening during the postpartum visit has increased from 2016 to 2021 in Utah, there is still room to increase consistency and frequency of screening services across clinics. Additionally, nurses have a unique opportunity to help patients in the perinatal period if they can receive adequate training because they are on the frontlines administering the screening tool. They can also be part of an IBH collaborative care model to bring physicians from different fields of expertise together to deliver optimal care to perinatally depressed women. Further research should be done to assess the usefulness of these recommendations and to evaluate the disparities in access to mental health services.
References
1. The American College of Obstetricians and Gynecologists. (2018). ACOG Committee opinion no. 757: Screening for perinatal depression. Obstetrics and Gynecology, 132(5), 208-212. https://doi.org/10.1097/aog.0000000000002927
2. Branquinho, M., Rodriguez-Munoz, M., Rodrigues Maia, B., Marques, M., Matos, M., Osma, J., Moreno-Peral, P., Conejo-Ceron, S., Fonseca, A., & Vousoura, E. (2021). Effectiveness of psychological interventions in the treatment of perinatal depression: A systematic review of systematic reviews and meta-analyses. Journal of Affective Disorders, 291, 294-306. https://doi.org/10.1016/j.jad.2021.05.010
3. Dagher, R. K., Bruckheim, H. E., Cople, L. J., Edwards, E., & White, D. B. (2021). Perinatal depression: Challenges and opportunities. Journal of Women’s Health, 30(2), 154-159. https://doi.org/10.1089/jwh.2020.8862
4. Huang, R., Yan, C., Tian, Y., Lei, B., Yang, D., Liu, D., & Lei, J. (2020). Effectiveness of peer support intervention on perinatal depression: A systematic review and meta-analysis. Journal of Affective Disorders, 276, 788-796. https://doi.org/10.1016/j.jad.2020.06.048
5. National Institute of Mental Health. (n.d.). Perinatal depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/perinatal-depression
6. Tripathy, P. (2020). A public health approach to perinatal mental health: Improving health and wellbeing of mothers and babies. Journal of Gynecology Obstetrics and Human Reproduction, 49(101747). http://dx.doi.org/10.1016/j.jogoh.2020.101747
7. Van Niel, M. S., & Payne, J. L. (2020). Perinatal depression: A review. Cleveland Clinic Journal of Medicine, 87(5), 273-277. https://doi.org/10.3949/ccjm.87a.19054
8. Centers for Disease Control and Prevention (CDC). (2022). Depression during and after pregnancy. Centers for Disease Control and Prevention. https://www.cdc.gov/reproductivehealth/features/maternal-depression/index.html
9. Valcarce K, Myrer R, & Garces J. (2022). Comparison of anxiety and depression among women who gave birth in Utah 2016-2020 using the Pregnancy Risk Assessment Monitory System (PRAMS). Utah Women’s Health Review. https://doi.org/10.26054/0d-46dz-sr1a
10. Talboys, S., Shoaf, K., Godin, S., & Hipol, F. (2020). Utah maternal and child health and children with special healthcare needs, statewide needs assessment 2020. University of Utah Division of Public Health. https://health.utah.gov/mch/documents/Utah%20Title%20V%20Needs%20Assessment%20Report/2020%20Utah%20MCH_CSHCN%20Needs%20Assessment%20(updated).pdf
11. Centers for Disease Control and Prevention (CDC). (2017). Pregnancy Risk Assessment Monitoring System (PRAMS): Phase 8 standard questions. Centers for Disease Control and Prevention. https://www.cdc.gov/prams/pdf/questionnaire/Phase-8-Standard-Core-Questions-508.pdf
12. Alba, B. M. (2021). Postpartum depression: A nurse’s guide. American Journal of Nursing, 121(7), 32-43. https://doi.org/10.1097/01.naj.0000756516.95992.8e
13. Raymond, N. C., Pratt, R. J., Godecker, A., Harrison, P. A., Kim, H., Kuendig, J., & O’Brien, J. M. (2014). Addressing perinatal depression in a group of underserved urban women: A focus group study. BMC Pregnancy and Childbirth, 14(336). https://doi.org/10.1186/1471-2393-14-336
14. Tebeka, S., Strat, Y. L., Higgons, S. D. P., Benachi, A., Dommergues, M., Kayem, G., Lepercq, J., Luton, D., Mandelbrot, L., Ville, Y., Ramoz, N., du Montcel, S. T., IGEDEPP Groups, Mullaert, J., & Dubertret, C. (2021). Prevalence and incidence of postpartum depression and environmental factors: The IGEDEPP cohort. Journal of Psychiatric Research, 138, 366-374. https://doi.org/10.1016/j.jpsychires.2021.04.004
15. Lomonaco-Haycraft, K. C., Hyer, J., Tibbits, B., Grote, J., Stainback-Tracy, K., Ulrickson, C., Lieberman, A., van Bekkum, L., & Hoffman, M. C. (2018). Integrated perinatal mental health care: A national model of perinatal primary care in vulnerable populations. Primary Health Care Research & Development, 20. https://doi.org/10.1017/S1463423618000348
16. Kang, P. S., Mohazmi, M., Ng, Y. M., & Liew, S. M. (2019). Nurses’ knowledge, beliefs and practices regarding the screening and treatment of postpartum depression in maternal and child health clinics: A cross-sectional survey. Malaysian Family Physician, 14(1), 18-25. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc6612276/
17. Ransing, R., Kukreti, P., Deshpande, S., Godake, S., Neelam, N., Raghuveer, P., Mahadevaiah, M., Kataria, D., Patil, S., Puri, M., & Padma, K. (2020). Perinatal depression–knowledge gap among service providers and service utilizers in India. Asian Journal of Psychiatry, 47. https://doi.org/10.1016/j.ajp.2019.10.002
18. Segre, L. S., Brock, R. L., O’Hara, M. W., Gorman, L. L., & Engeldinger, J. (2011). Disseminating perinatal depression screening as a public health initiative: A Train-the-Trainer approach. Maternal and Child Health Journal, 15(6), 814-821. https://doi.org/10.1007/s10995-010-0644-1
19. Utah Department of Health and Human Services (UDHHS). (2022). Public Health Indicator Based Information System (IBIS): Utah’s public health data resource. Utah Department of Health and Human Services. https://ibis.health.utah.gov/ibisph-view/
20. Chen, J., Cross, W. M., Plummer, V., Lam, L., Sun, M., Qin, C., & Tang, S. (2019). The risk factors of antenatal depression: A cross‐sectional survey. Journal of Clinical Nursing, 28, 3599-3609. https://doi.org/10.1111/jocn.14955
21. Wang, T. H., Tzeng, Y. L., Teng, Y. K., Pai, L. W., & Yeh, T. P. (2022). Evaluation of psychological training for nurses and midwives to optimise care for women with perinatal depression: a systematic review and meta-analysis. Midwifery, 104(103160). https://doi.org/10.1016/j.midw.2021.103160
22. Utah Women and Newborns Quality Collaborative (UWNQC), Maternal Mental Health Committee. (2022). Utah’s maternal mental heath toolkit: Resources for anyone working with perinatal parents and their children. UWNQC. https://mihp.utah.gov/mmhtoolkit
23. Miller, E. S., Jensen, R., Hoffman, M. C., Osborne, L. M., McEvoy, K., Grote, N., & Moses-Kolko, E. L. (2020). Implementation of perinatal collaborative care: A health services approach to perinatal depression care. Primary Health Care Research & Development, 21(e30), 1-9. https://doi.org/10.1017/S1463423620000110
24. Bayrampour, H., Hapsari, A. P., & Pavlovic, J. Barriers to addressing perinatal mental health issues in midwifery settings. Midwifery, 59, 47-58. https://doi.org/10.1016/j.midw.2017.12.020
Citation
Waechtler L and Talboys S (2024). Perinatal depression trends in Utah and the role of nurses and integrated behavioral health professionals. Utah Women’s Health Review. doi: 10.26054/d-k9mp-4mw1

