Infertility is typically defined as a lack of pregnancy among couples who have had one year of sexual intercourse without using contraception. Worldwide, millions of couples suffer from infertility. Population-based surveys from the United States and Great Britain indicate that between 8 and 10% of women suffer from impaired fertility; however, as far as we know, less than half of women seek medical treatment for this condition [1-2]. Couples with infertility may experience emotional distress and devastation when their childbearing desires and expectations are not realized. Infertility may also be an indicator of underlying health problems that can lead long-term consequences such as heart disease or cancer [3-4]. In addition, couples who receive infertility treatment have increased risk for multiple gestations, preterm birth, birth defects, growth restricted infants, and possibly children with developmental delays, perhaps depending upon the type of treatment received [5-8]. Thus, infertility is an important public health issue for couples in Utah and worldwide.
Despite the importance of infertility, there has been little population-based assessment of its incidence, treatment, and outcomes. In Utah, assessment of time to pregnancy and utilization of infertility services among women who have had a live birth was incorporated as of 2004 as part of the Pregnancy Risk Assessment and Monitoring System (PRAMS) [9]. PRAMS is an ongoing, population-based surveillance system designed to identify and monitor maternal health and behaviors before, during, and after pregnancy. Surveys are conducted in both English and Spanish. A stratified random sample of women who have delivered a live-born infant in Utah are identified and contacted 2-6 months postpartum with over-sampling of women with lower education levels and women who have delivered low birth weight infants. The data presented in this report are from the 2004 – 2005 PRAMS surveys, and include responses from 3789 questionnaires, weighted to represent the 98,636 women with births that occurred in Utah in 2004 and 2005 (a weighted response rate of 88.5% was achieved). Some of the questions are asked only to women who reported they were trying to get pregnant at the time of the conception leading to the current pregnancy; after weighting, the data represent the 57,806 Utah women (60.0%) who were trying to get pregnant and who delivered a live born infant 2004/2005. Data from three PRAMS questions about fertility are included in this report. These questions are as follows:
Data from three PRAMS questions about fertility are included in this report. These questions are as follows:
- Did you receive treatment from a doctor, nurse, or other health care worker to help you get pregnant with your new baby? [This question was only asked to women who reported that they were trying to get pregnant at the time of the current pregnancy.]
- Did you use any of the following treatments during the month you got pregnant with your new baby?(Check all that apply) [This question was only asked to women who reported that they were trying to get pregnant at the time of the current pregnancy.]
a. Fertility-enhancing drugs prescribed by a doctor (fertility drugs include Clomid, Serophene, Pergonal, or other drugs that stimulate ovulation)
b. Artificial insemination or intrauterine insemination (treatments in which sperm, but NOT eggs, were collected and medically placed into a woman’s body)
c. Assisted reproductive technology (treatments in which BOTH a woman’s eggs and a man’s sperm were handled in the laboratory, such as in vitro fertilization [IVF], gamete intrafallopian transfer [GIFT], zygote inrafallopian transfer [ZIFT], intracytoplasmic sperm injection [ICSI], frozen embryo transfer, or donor embryo transfer)
d. Other medical treatment - How many months had you been trying to
a. 0 to 3 month
b. 4 to 6 month
c. 7-12 months
d. 13-24 months
e. More than 24 months
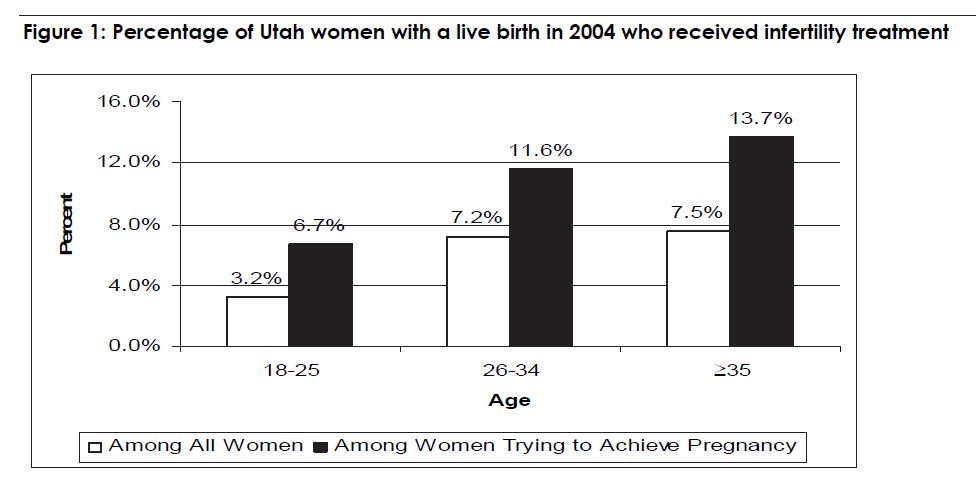
In 2004 – 2005, 5.5% of all women giving birth in Utah received some type of infertility treatment. Restricted to women who reported they were trying to get pregnant, 10.0% of women utilized infertility treatment. The proportion of women receiving infertility treatment increased with age (see Figure 1). As expected, the proportion of births complicated by twins was higher among women who received infertility treatment. Approximately 7.2% of Utah women who were trying to get pregnant and used infertility treatment gave birth to twins, in comparison with 1.3% of women who were trying to get pregnant and did not utilize infertility treatment. In 2004 – 2005, nearly 40% of multiple births in Utah occurred in women who were using infertility treatment.
The most common type of infertility treatment used by Utah women in 2004/05 was fertility enhancing drugs (60%). In contrast, 11.7% received assisted reproductive technology (ART) (see figure 2). “Other” types of treatment, used by 18.7% of women, include drugs such as glucophage or surgical treatments for conditions such as endometriosis.
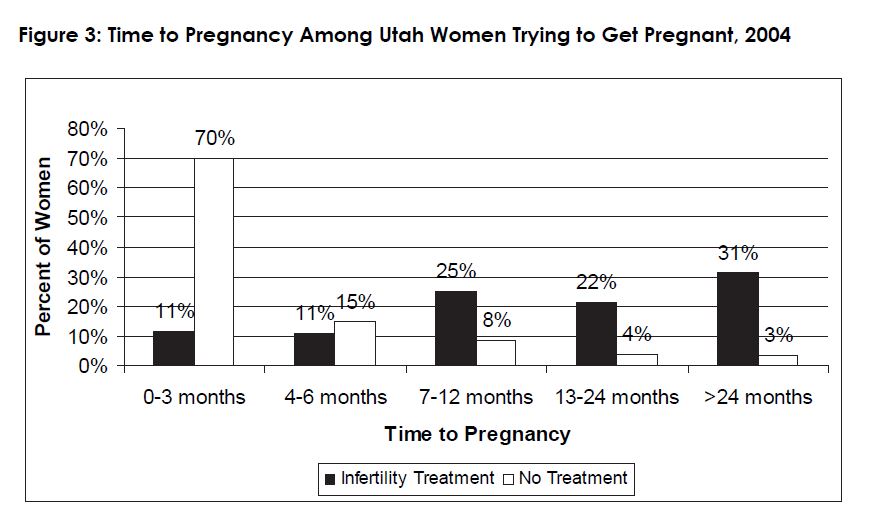
Among those who did not receive infertility treatment, 85% reported that they had been trying to get pregnant for 6 months or less, and 93.4% had been trying for 12 months or less. This is consistent with other studies of time to pregnancy.10 Among women who were trying to get pregnant and received infertility treatment, 47% had a self-reported time to pregnancy of 12 months or less (see figure 3). This is an interesting time to pregnancy distribution because current guidelines for infertility treatment recommend that couples wait at least 12 months before initiating treatment, unless the woman is 35 years of age or older. Unfortunately, we are unable to examine the time to pregnancy data among women age ≥ 35 who utilized infertility treatment due to sample size limitations.
There are several limitations to this analysis. The PRAMS data are only collected on women who have a pregnancy resulting in a live birth. Thus, women with infertility who never become pregnant or women who suffer a miscarriage will not be included. This results in an underestimation of the true impact of infertility on Utah women. Further, because of the small sample size, we were unable to stratify results by race/ethnicity. Although the information on utilization of infertility treatment is only collected for women who report that they were trying to get pregnant, it seems unlikely that there would be many women who received treatment but did not report trying to get pregnant. Finally, these data capture self-reported infertility treatment and time to pregnancy and are not validated by medical record reviews. Women’s interpretations of questions about infertility treatment may vary. In particular, there is uncertainty of the interpretation of the time to pregnancy question. Although it is a standard question used in retrospective surveys to assess time to pregnancy, in this PRAMS survey, it immediately follows the question about receiving treatment. Therefore, the interpretation of this question by women who received treatment could be how long they tried to get pregnant prior to treatment, during treatment, or both. However, the interpretation who did not receive treatment remains relatively straightforward.
Despite these limitations, the PRAMS data give us important insight into infertility in Utah.
Infertility treatment is relatively common among Utah women, and is involved in over 5% of births. The utilization of infertility treatment is more common among older women. Twins occur frequently among women who use infertility treatment. Fertility enhancing drugs are the most common type of infertility treatment used by Utah women. The atypical time to pregnancy distribution among women who received infertility treatment indicates that treatment may be initiated as early as 1-3 months after couples begin trying to become pregnant. A delay in treatment initiation may result in similar pregnancy outcomes for many of these women, while reducing the risks of multiple gestations and the associated poor neonatal outcomes that may occur with the utilization if infertility treatment. Further longitudinal research is needed to understand the optimal timing of fertility treatment, and the long term consequences of infertility treatment on neonatal outcomes and development.

References
- Mosher WD, Pratt, WF. Fecundity and infertility in the United States, 1965-88.Advance data from vital and health statistics. No. 192. Hyattsville, MD.: Public Health Service, 1990 (vol DHHS publication no. (PHS) 91-1250).
- Chandra, A., G. Martinez, et al. (2005). Fertility, family planning, and reproductive health of U.S. women: Data from the 2002 National Survey of Family Growth. NSFG Statistics. Atlanta, GA, CDC, NCHS, Hyattsville, MD. 23: 174.
- Dahlgren E, Janson PO, Johansson S, Lapidus L, Oden A. Polycystic ovary syndrome and risk for myocardial infarction Evaluated from a risk factor model based on a prospective population study of women. Acta Obstet Gynecol Scand. Dec 1992;71(8):599-604.
- Brinton LA, Westhoff CL, Scoccia B, et al. Causes of infertility as predictors of subsequent cancer risk. Epidemiology. Jul 2005;16(4):500-507.
- Jackson RA, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol 2004;103(3):551-63.
- Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with use of assisted reproductive technology. The New England journal of medicine 2002;346(10):731-7.
- Schieve LA, Rasmussen SA, Reefhuis J. Risk of birth defects among children conceived with assisted reproductive technology: providing an epidemiologic context to the data. In: Fertil Steril; 2005:1320-4; discussion 7.
- Stromberg B, Dahlquist G, Ericson A, Finnstrom O, Koster M, Stjernqvist K. Neurological sequelae in children born after in-vitro fertilisation: a population-based study. Lancet 2002;359(9305):461-5.
- Utah Department of Health. Utah PRAMS Data Book 2002-2003. Available online at: http://health.utah.gov/rhp/pdf/ 02_03_Data_Book.pdf. Accessed January 29, 2007.
- Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod 2003;18(9):1959-66.