Table of Contents
Background
Postpartum depressive symptoms (PDS) can range from the “baby blues”—when for a short period of time after childbirth, a mother experiences mood swings, anxiety, sadness, and/or appetite/sleeping problems—to postpartum depression (PPD)—which involves similar signs and symptoms but is experienced more intensely and for a longer period of time, and may interfere with a mother’s ability to care for her baby and herself. Up to 80% of women in the United States may experience transient PDS, and up to 12% are estimated to experience PPD (Ko et al., 2017). If left untreated, moderate to severe PPD has been linked with lower rates of breastfeeding duration and initiation, impairment of mother-infant bonding, and delayed social and cognitive development of offspring (Ko et al., 2017).
Timing is the only aspect that distinguishes PDS or PPD from other types of depression. The American Psychiatric Association defines PPD as a major depressive episode with onset in pregnancy or within 4 weeks after delivery (American Psychiatric Association, 2015). A new mother who experiences three or more out of the following symptoms in the same period, in addition to depressed mood and loss of interest or pleasure, would be diagnosed with PPD:
- Change in weight or appetite. Weight: 5 percent change over 1 month;
- Insomnia or hypersomnia;
- Psychomotor retardation or agitation (observed);
- Loss of energy or fatigue;
- Feelings of worthlessness or guilt;
- Impaired concentration or indecisiveness;
- Recurrent thoughts of death or suicidal ideation or attempt.
Given the serious consequences of postpartum depression and its relatively high prevalence, a developmental Healthy People 2020 goal is to reduce the proportion of women who experience PDS after delivering a live birth. Healthy People 2020 defines this as a developmental objective since the condition lacks national baseline data. Consequently, no technical specifications for improvement are specified; however, a nationally representative data source that can provide a tracking point exists. Furthermore, it is acknowledged that this is an important concern deserving of monitoring for improvement (Office of Disease Prevention and Health Promotion).
Given evidence supporting that PDS and PPD are treatable via pharmacologic therapy and/or behavioral interventions (Ko et al., 2012), the key to reducing morbidity and mortality associated with this maternal condition is proper screening, diagnosis, and treatment of at-risk mothers. Research conducted within the last decade indicates that nearly 60% of new mothers with depressive symptoms do not receive a clinical diagnosis and 50% of women with a clinical diagnosis do not receive any treatment (Ko et al., 2012). Consequently, several professional women’s health groups, including the American College of Obstetricians and Gynecologists, recommend that providers screen for depression at least once during pregnancy or postpartum. Some even advocate the need to screen pre-conceptionally, given that women with a history of depression have a two-fold increased risk of suffering from PPD (Gauthreaux et al., 2017).
Our objective in this data snapshot is to provide recent Utah statistics on prevalence of preconception and prenatal/postpartum depression screening and diagnosis, using the Pregnancy Risk Assessment Measurement’s Survey (PRAMS) for Utah. Additionally, we aim to compare current Utah statistics with those of the past and for the rest of the United States.
Data
Utah Pregnancy Risk Assessment Monitoring System (UT-PRAMS) Methodology:
Participants contributing responses for this data snapshot were mothers who participated in the Utah Pregnancy Risk Assessment Monitoring System (UT-PRAMS) between 2012 and 2014. Two questions were specifically related to PDS: 1) “Since your new baby was born, how often have you felt down, depressed, or hopeless?”; and 2) “Since your new baby was born, how often have you had little interest or little pleasure in doing things?” For both questions, women were given options of “Always”, “Often”, “Sometimes”, “Rarely”, or “Never”. As per the Centers for Disease Control (CDC) PRAMS methodology, we classified any woman who answered “Always” or “Often” as having PDS. Sociodemographic, lifestyle, and health history questions also make up the PRAMS questionnaire, in addition to inquiries about past history of depression and whether any health care provider discussed with them what they should do if they felt any depressive symptoms during or after their baby was born.
Women who answered either question in regards to PDS were included in the analysis
(n=4328/4378, 99%). Descriptive characteristics including socio-demographic, psychosocial, and health factors of Utah mothers by PDS status (yes/no) were calculated by chi square or t-tests as appropriate, taking into account the stratified random sampling in the analyses. Key risk factors for Utah mothers were evaluated via adjusted Poisson regression to generate prevalence ratios (PR) and 95% confidence intervals. Analyses were completed using SAS version 9.4 (SAS Institute, Inc.).
Utah Pregnancy Risk Assessment Monitoring System (UT-PRAMS) Results:
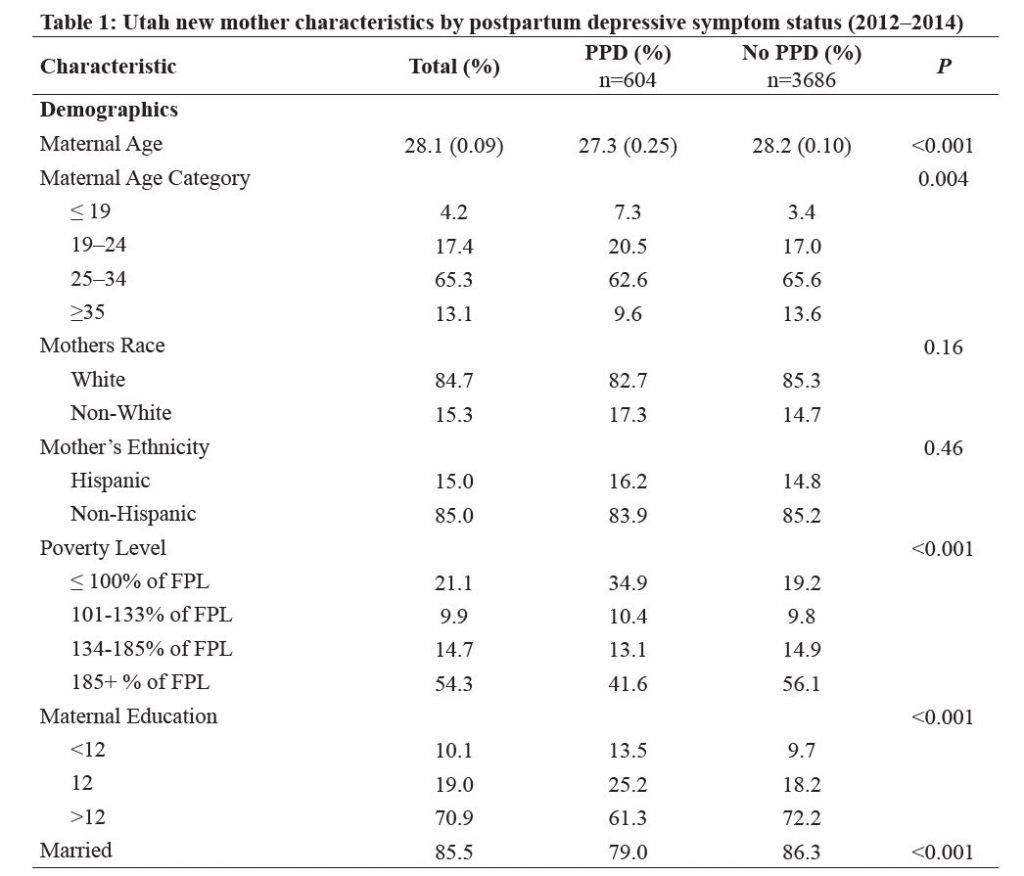


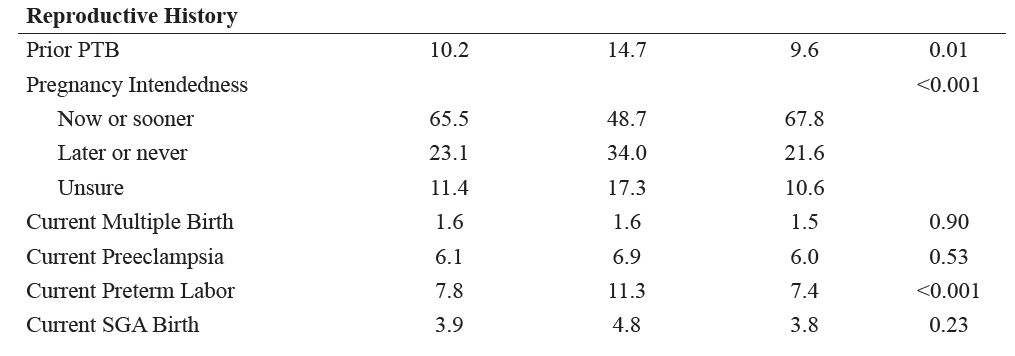

Prevalence of PDS among Utah women, 2012–2014, was 12.0%. In regards to demographic and health characteristics, women who experienced PDS compared to those who did not were more likely to be younger (27.3 vs 28.2 years), lower income (34.9% vs 19.2% ≤ 100% of Federal Poverty Level [FPL]), higher body mass index (BMI) (26.1 vs 25.3), to report a prior-to-pregnancy diagnosis of hypertension (3.8% vs 1.9%) and depression (29.0% vs 7.3%), and to report a 3-months-prior-to-pregnancy history of asthma (10.3% vs 6.9%), anemia (12.4% vs 7.1%), and/or anxiety (32.7% vs 11.4%) (Table 1). In regards to psychosocial and lifestyle factors, women with versus without PDS were more likely to report partner abuse prior to and during pregnancy (3.9% vs 1.3% and 4.0% vs 1.1%, respectively), 3-months-prior-to-pregnancy smoking (15.8% vs 8.4%) or alcohol (29.4% vs 23.2%) exposure, and presence of higher partner (43.7% vs 18.5%), traumatic (22.5% vs 10.1%), financial (57.4% vs 47.4%), or emotional (35.9% vs 27.6%) life stressors. Finally, women with versus without PDS were more likely to have a current (11.3% vs 7.4%) or prior (14.7% vs 9.6%) preterm birth (PTB) and more likely to have an unintended pregnancy (34.0% vs 21.6%).
In the adjusted analyses, after taking into account mother’s age, race, ethnicity, and BMI, the statistically significant predictors of PDS included being ≤100% of federal poverty level (PR: 1.48 [95% CI: 1.21, 1.82]), having had a prior diagnosis of depression or anxiety (PR 2.09 [95% CI: 1.58, 2.77]; PR 1.60 [95% CI: 1.22, 2.1], respectively), experiencing partner-related or traumatic-related stress (PR 1.76 [95% CI: 1.41, 2.20]; PR 1.24 [95% CI: 0.98, 1.55], respectively), and having a preterm birth infant for the most recent pregnancy (i.e., 2–4 months prior) (PR:1.35 [95% CI: 1.08, 1.69]) (Figure 1). None of the other factors listed in Table 1, including mother’s age, race, ethnicity, and BMI, significantly predicted a woman’s risk of PDS.
Current State of PDS in Utah compared to the Past and to the Rest of the United States In line with the majority of the US, which has witnessed a statistically significant decline in PDS from 2004 to 2012 among 13 states (with data for all periods), PDS in Utah has dropped from 14.8% in 2004 to 12.4% in 2008 to 11.3% in 2012 (P for trend = 0.01) (Ko et al., 2017). Among the 27 states participating in the 2012 PRAMS survey, Utah’s 11.3% PDS prevalence ranks 14th in the US (average: 11.5%; range 8.0 to 20.1). However, the 2013 to 2014 UT-PRAMS data do not support a continuing decline, with the prevalence going up to 12.5% in 2013 and 12.3% in 2014.
In terms of characteristics significantly associated with PDS, Utah was similar to the rest of the US, with PDS being higher in younger, unmarried, less educated, more highly stressed women who gave birth to a preterm infant. (Ko et al., 2017) What our results show for the UT-PRAMS 2012–2014 data is that the risk factors that are most predictive of PDS in Utah, after taking into account maternal age and race/ethnicity include 1) living below 100% of the federal poverty level; 2) a prior depression or anxiety diagnosis; 3) experiencing partner- or traumatic-related stress; and 4) having a preterm infant.
Conclusion
Our findings from the UT-PRAMS 2012–2014 survey highlight that approaching PDS truly requires a multidisciplinary approach, particularly in the domains of social, emotional, and financial support. The CDC points to several factors that may be linked to the reduced prevalence of PDS in the US from 2004 to 2012, including reduction in teen births, preterm births, and self-reported stressful life events as well as an increase in antidepressant prescriptions for pregnant women (Ko et al., 2017). Our findings from UT-PRAMS 2012–2014 indicate that new mothers who have a prior history of depression and anxiety are at significant increased risk for PDS and thus should be a subgroup who receive extra attention by healthcare providers in terms of appropriate screening, referral, and treatment (Practice, 2015) (Earls et al., 2010). Utah women who have experienced partner or traumatic-related stressors or who are in the lowest income brackets are also at high risk for PDS and deserve special consideration.
Finally, it is important to note that ~30% of women reported that their prenatal doctor, nurse, or other health care worker never talked with them during one of their prenatal care visits about what to do if they felt depressed or suffered from physical abuse during or after their pregnancy. While we found no difference in PDS risk by having or not having these discussions, professional women’s health organizations have come up with new strategies that may make these discussions more effective. Strategies include using validated screening tools (American College of Obstetricians and Gynecolo-gists, 2015) and extending maternal mental health screening to postpartum period during well-baby and/or primary care visits (Earls et al., 2010; Ko et al., 2017; Practice, 2015). Another useful resource for both health professionals and mothers/families is the Utah Maternal Health Collaborative, a state chapter of Postpartum Support International. Founded in September 2014, this is an all-volunteer organization made up of several hundred community members including survivors of maternal depression as well as healthcare providers (http://www.utahmmhc.org).
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders, (5th ed.) (DSM-5). Washington, DC: American Psychiatric Publishing.
- Earls, M. F., (2010). Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics, 126(5), 1032-1039.
- Gauthreaux, C., Negron, J, Castellanos, D., Ward-Peterson, M., Castro, G., Rodriguez de la Vega, P. & Acuña, J. M. (2017). The association between pregnancy intendedness and experiencing symptoms of postpartum depression among new mothers in the United States, 2009 to 2011: A secondary analysis of PRAMS data. Medicine, 96(6), e5851.
- Healthy People 2020. Washington, DC. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Maternal, Infant and Child Health: Postpartum Health and Behavior. Available from https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives. Accessed May 1, 2019
- Ko, J. Y., Farr, S. L., Dietz, P. M., & Robbins, C. L. (2012). Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005-2009. J Womens Health (Larchmt), 21(8), 830-836.
- Ko, J. Y., Rockhill, K. M., Tong, V. T., Morrow, B. & Farr, S. L. (2017). Trends in Postpartum Depressive Symptoms – 27 States, 2004, 2008, and 2012. MMWR. Morbidity and Mortality Weekly Report, 66(6), 153-158.
Citation
Elmer A, McEwan M, Schliep K. (2019). Data Snapshot: Postpartum Depression. Utah Women’s Health Review. doi: 10.26054/0KYY9AQVJ2.

