Table of Contents
Background
Throughout the world, individuals have experienced multiple adverse physical outcomes as a result of the COVID-19 pandemic; in addition, they have been impacted by unfavorable mental health outcomes arising from the pandemic.1 Pregnant women are especially vulnerable to mental health distress during times of national crises.2 Depression and anxiety during pregnancy can have adverse effects on both mother and child. In one study, maternal depression during pregnancy was associated with inflammation.3 Inflammation during pregnancy has been shown to be associated with increased risk of mental illness or neurological development problems in children.4 In another study, among women with depression during pregnancy, rates of preeclampsia, premature membrane rupture, preterm delivery, cesarean section, intrauterine fetal death, and intrauterine fetal growth restriction were elevated compared to women who did not report depression during pregnancy.5 Furthermore, maternal depression during pregnancy has been shown to be associated with lower child cognitive development.6 Given the importance of mental health during pregnancy to help prevent adverse health outcomes, the objective of this data snapshot is to determine how prevalence of anxiety and depression among pregnant women in Utah have changed over time, notably before and during the COVID-19 pandemic, and to describe the resources available to pregnant women to address mental health.
Data
The Pregnancy Risk Assessment Monitory System (PRAMS) is an ongoing, population-based surveillance project coordinated by the Centers for Disease Control and Prevention (CDC). Through a collaboration of the CDC and the Utah Department of Health (UDOH), Utah is 1 of 47 states that collect PRAMS data. PRAMS surveillance in Utah began in 1999 with the intent to monitor maternal and child health indicators. Based on Utah birth certificates, approximately 200 new mothers are randomly selected for participation each month. Following a protocol developed by the CDC that utilizes mail and telephone questionnaires, approximately 60 percent of new mothers who are randomly selected respond. The responses are weighted to be representative of all women who have live births in Utah.7 The data included in this snapshot was collected between January 1, 2016, and December 31, 2020.
The standardized approach of the PRAMS data collection is a strength, as PRAMS’ stratified random sampling means that women from some groups are sampled at higher rates to ensure adequate data are available for target populations. UT-PRAMS oversamples women of lower education levels and infant birth weight to generate data on at-risk populations. The CDC-standardized PRAMS questionnaire also allows for comparisons between states and across multiple years. Another strength of PRAMS is the breadth and depth of collected data. The questionnaire seeks information on demographics and preconception-, pregnancy-, and postpartum health-related behaviors, attitudes, and health outcomes. However, PRAMS data are self-reported and may be subject to social desirability and recall biases.
Results
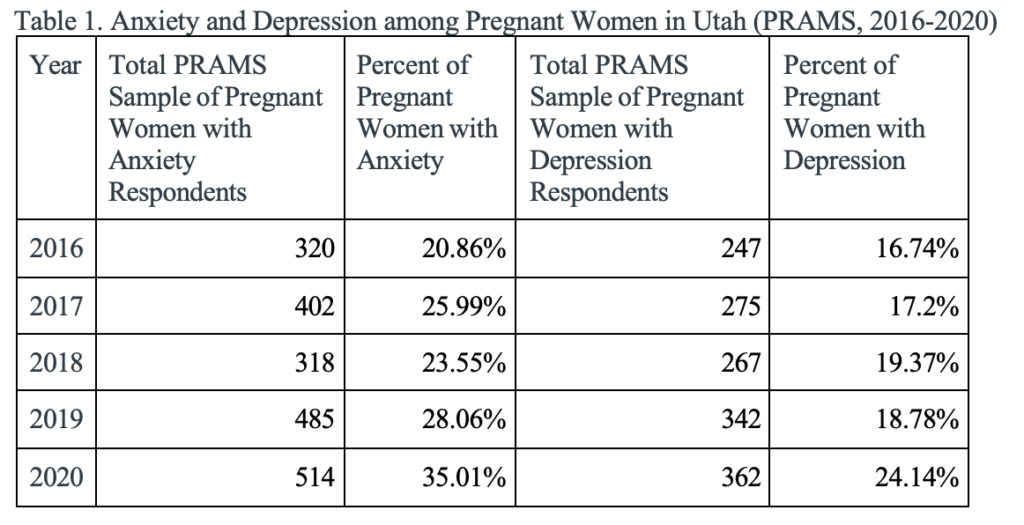
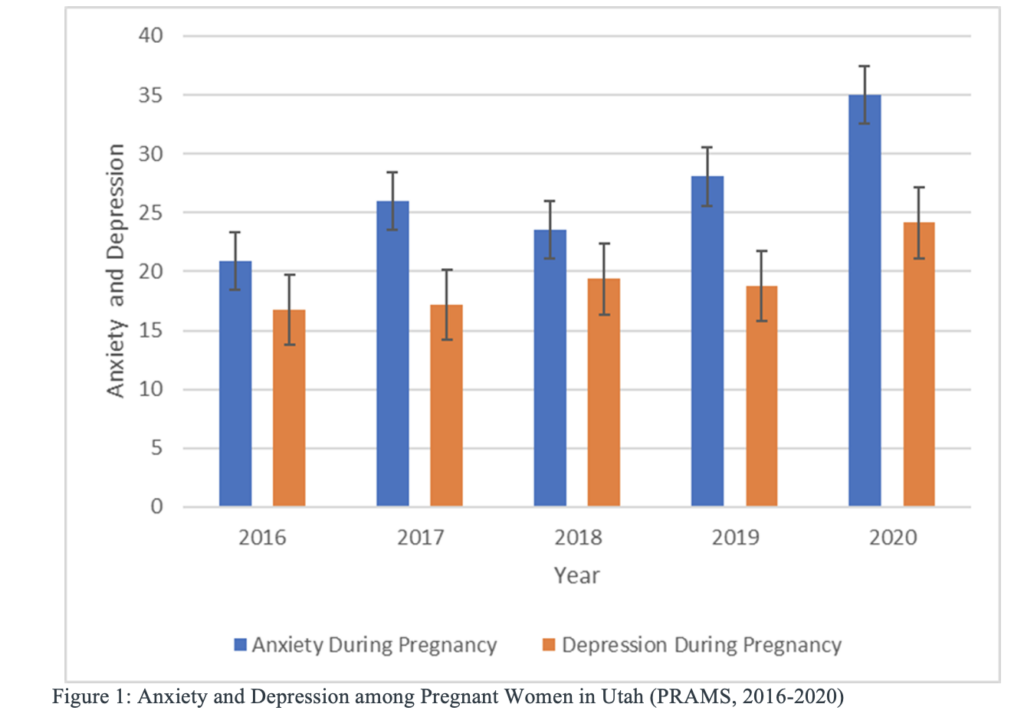
Depression and anxiety rates among pregnant women in Utah rose notably between 2016 and 2020 (Table 1 and Figure 1). Rates of anxiety during pregnancy had an absolute increase of more than 14 percent (20.9% to 35.0%), and depression increased by more than 7 percent (16.7% to 24.1%) during this period. The confidence intervals for rates of both anxiety and depression do not overlap between 2019 and 2020. This increase has a devastating impact on the emotional and physical health of mothers and their children. While it is immediately unclear why rates of anxiety and depression during pregnancy were rising between 2016 and 2020, the COVID-19 pandemic could partially explain the increases in more recent years, from 2019 to 2020 (7.0% absolute increase in anxiety, and 5.4% absolute increase in depression). In a study with Canadian women conducted for the same time period, increased anxiety and depression were observed during pregnancy compared to pre-pandemic pregnancy cohorts. Several reasons were cited for this increase related to the pandemic, including social isolation, relationship stress, less access to prenatal care, and concern about the threat of COVID-19 to the health of the mother and baby.8
Conclusion
Rates of anxiety and depression among pregnant women in Utah have been increasing since 2016. This is in line with findings from other US states of pregnant women who have shown a more pronounced increase in anxiety and depression during the pandemic compared to before the pandemic 1 Anxiety and depression during pregnancy not only negatively affect the emotional and physical health of the mother, but also can negatively impact the health of the baby. It is fair to speculate that increased rates of depression and anxiety also cause an increase in the adverse health outcomes discussed above, such as rates of preeclampsia, premature membrane rupture, preterm delivery, cesarean section, intrauterine fetal death, intrauterine fetal growth restriction, and lower cognitive development of the infant.
There are a few recent studies that have addressed what factors may help decrease the risk of anxiety and depression during pregnancy, specific to the context of the COVID-19 pandemic. Lebel, et al., found that increased social support and increased exercise were protective factors.8 Similarly, Khourry, et al., found that social support was associated with lower amounts of mental health problems during pregnancy.10 More research is needed, however, on why anxiety and depression during pregnancy may be increasing and what pregnant women and their healthcare providers can do to help reduce the risk of experiencing them in addition to resources currently available. Healthcare providers should screen for anxiety and depression at least one time during pregnancy. Treatments are available, including psychotherapy or antidepressants.9 UDOH offers a Maternal Mental Health Referral Network, which allows individuals to search for mental health providers throughout Utah by county, provider type, insurance, and specialty.11 The University of Utah also has a dedicated webpage with information about mental health problems during and after pregnancy and maternal mental health services .12 The Utah Women and Newborns Quality Collaborative works with providers statewide to make recommendations on education, screening, detection, and response protocols.13 Other resources are available, such as the Emily Effect, which allows individuals to share their stories relating to mental health during and after pregnancy.14 Regardless of their experience during pregnancy, pregnant women with mental health concerns should not hesitate to reach out to their healthcare providers.
Acknowledgements
Data were provided by the UT-PRAMS, a project of the UDOH, the Office of Vital Records and Health Statistics of the UDOH, and the CDC of the US Health and Human Services Department. This report does not represent the official views of the CDC or UDOH.
References
- López-Morales H, Del Valle MV, Canet-Juric L, et al. Mental health of pregnant women during the COVID-19 pandemic: A longitudinal study. Psychiatry Res. 2021;295:113567. doi:10.1016/j.psychres.2020.113567
- Alfayumi-Zeadna S, Bina R, Levy D, Merzbach R, Zeadna A. Elevated perinatal depression during the COVID-19 pandemic: A national study among Jewish and Arab Women in Israel. J Clin Med. 2022 Jan 11;11(2):349. doi: 10.3390/jcm11020349. PMID: 35054043; PMCID: PMC8778708.
- Lahti-Pulkkinen M, Girchenko P, Robinson R, et al. Maternal depression and inflammation during pregnancy. Psychol Med. 2020;50(11):1839-1851. doi:10.1017/S0033291719001909
- Rudolph MD, Graham AM, Feczko E, et al. Maternal IL-6 during pregnancy can be estimated from newborn brain connectivity and predicts future working memory in offspring. Nat Neurosci. 2018;21(5):765-772. doi:10.1038/s41593-018-0128-y
- Khanghah AG, Khalesi ZB, Hassanzadeh Afagh R. The importance of depression during pregnancy. JBRA Assist Reprod. 2020;24(4):405-410. doi:10.5935/1518-0557.20200010
- Urizar GG, Muñoz RF. Role of maternal depression on child development: A prospective analysis from pregnancy to early childhood. Child Psychiatry Hum Dev. Published online March 1, 2021. doi:10.1007/s10578-021-01138-1
- Utah PRAMS. Maternal and Infant Health Program. Accessed March 22, 2022. https://mihp.utah.gov/pregnancy-and-risk-assessment. Includes IBIS-PH – Pregnancy Risk Assessment Monitoring System (PRAMS) Query Module. Public Health Indicator Based Information System (IBIS). Accessed April 1, 2022. https://ibis.health.utah.gov/ibisph-view/query/selection/prams/PRAMSSelection.html
- Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5-13. doi:10.1016/j.jad.2020.07.126
- Mayo Clinic Staff. Depression during pregnancy: You’re not alone. Mayo Clinic. Published January 25, 2022. Accessed March 22, 2022. https://www.mayoclinic.org/healthy- lifestyle/pregnancy-week-by-week/in-depth/depression-during-pregnancy/art-20237875
- Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. COVID-19 and mental health during pregnancy: The importance of cognitive appraisal and social support. J Affect Disord. 2021;282:1161-1169. doi:10.1016/j.jad.2021.01.027
- Maternal Mental Health Provider Network. MHRN. Accessed March 22, 2022. https://maternalmentalhealth.utah.gov/
- Maternal Mental Health Services. Huntsman Mental Health Institute. Accessed March 22, 2022. https://healthcare.utah.edu/hmhi/treatments/maternal-mental-health/index.php
- UWNQC. Maternal and Infant Health Program. Accessed March 22, 2022. https://mihp.utah.gov/uwnqc/maternal-mental-health
- The Emily Effect. Accessed March 22, 2022. https://theemilyeffect.org/
Citation
Valcarce K, Myrer R, and Garces J. (2022). Comparison of Anxiety and Depression among Women Who Gave Birth in Utah 2016-2020 Using the Pregnancy Risk Assessment Monitory System (PRAMS). Utah Women’s Health Review. doi: 10.26054/0d-46dz-sr1a

